Diabetic Foot Pain Symptoms
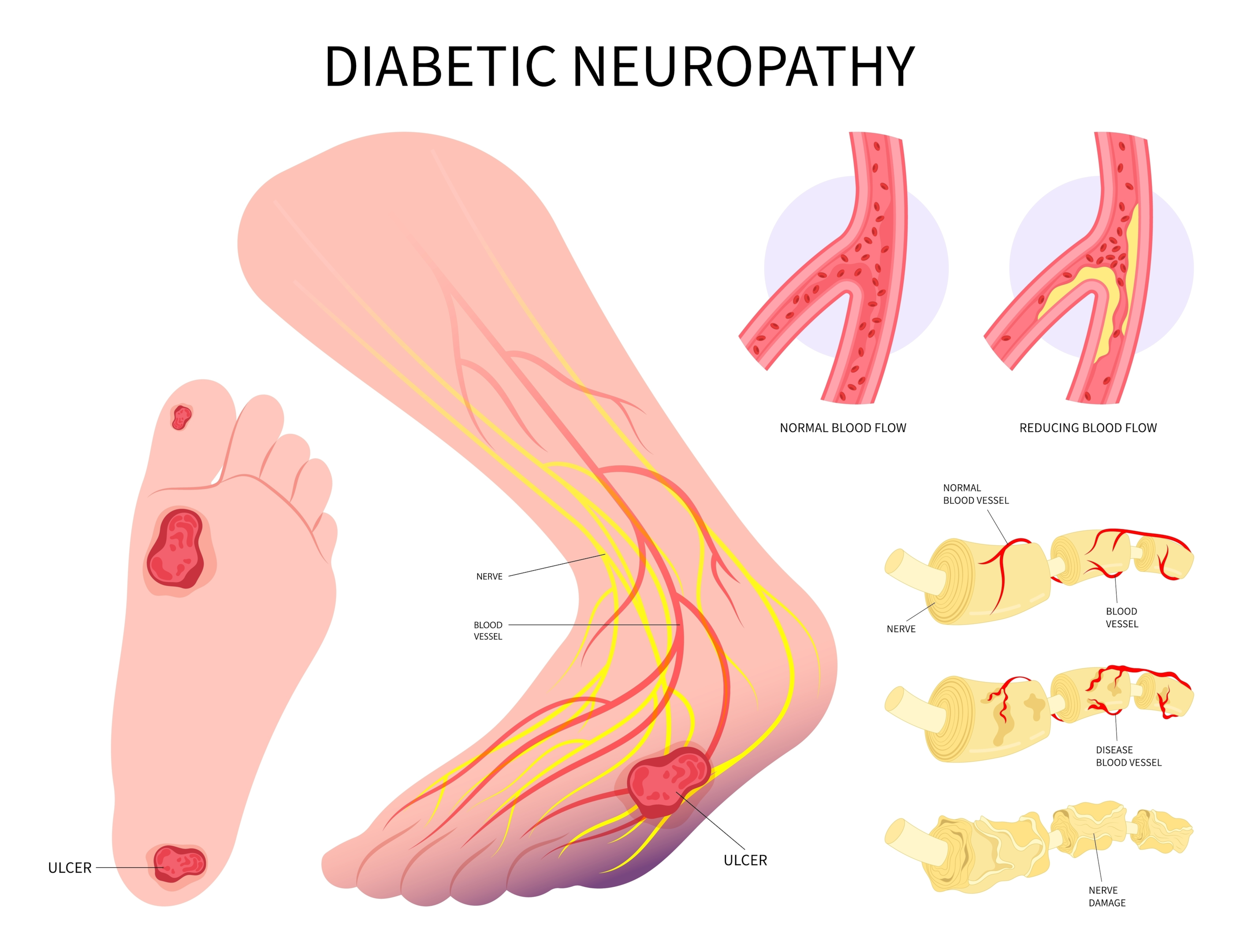
Diabetic neuropathy is a severe health issue affecting many people with diabetes. It is nerve damage due to high blood sugar levels, affecting various body parts, especially the feet. For people living with this condition, understanding the symptoms of diabetic foot pain and diabetic neuropathy is crucial to managing the situation effectively and preventing further complications.
Understanding diabetic neuropathy begins with knowing that our body’s nerves are like electric cables that transmit signals from one area to another. In diabetic neuropathy, these cables are damaged, disrupting the normal flow of movements. The feet and legs are often the first to be affected, resulting in foot problems caused by diabetes, such as numbing, tingling, or burning sensations.
Living with diabetic neuropathy can be a constant struggle, but with the proper knowledge, you can take control of your health. Monitoring your symptoms, maintaining a healthy lifestyle, and working closely with your healthcare provider is essential. The journey may be challenging, but remember that you are not alone.
Understanding the Signs and Symptoms of Diabetic Foot Problems
The symptoms of diabetic foot pain can vary from person to person, depending on the severity of the nerve damage. Some people experience mild symptoms, while others have severe, debilitating pain. Knowing these symptoms can help in early detection and management regardless of the intensity.
One of the most common symptoms is a burning or sharp pain in the feet. This pain is often worse at night and may disrupt sleep. Other signs include extreme sensitivity to touch, where even the weight of a bedsheet can cause discomfort, and a loss of balance or coordination, mainly when walking.
Furthermore, some people may experience muscle weakness in their feet. This can result in difficulty walking or performing routine activities like climbing stairs. It’s common to have numbness or insensitivity to pain or temperature changes, which can increase the risk of injury. It is crucial to monitor these symptoms closely and seek medical help if they worsen over time.
Diabetic Foot Pain: Causes and Relief
The primary cause of diabetic foot pain is high blood sugar levels over a prolonged period, leading to nerve damage. The elevated and uncontrolled blood sugar levels damage the small blood vessels that supply oxygen and nutrients to the nerves, leading to poor blood flow. This, in turn, leads to diabetic neuropathy.
Other contributing factors include nerve inflammation, genetic factors, and smoking. Each of these affects the blood flow, which leads to more foot complications.
To find relief from diabetic foot pain, managing your blood sugar levels effectively is essential. This can be achieved through a healthy diet, regular exercise, and medication if prescribed by your doctor. Additionally, pain relievers, anti-seizure drugs, and antidepressants can also be used to up blood glucose and manage the pain.
Another crucial aspect of managing diabetic foot pain is caring for your feet. This includes wearing comfortable shoes, keeping your feet clean and dry, and regularly inspecting your feet for any signs of injury or infection. Regular foot massages can also help in alleviating the pain and improving circulation.
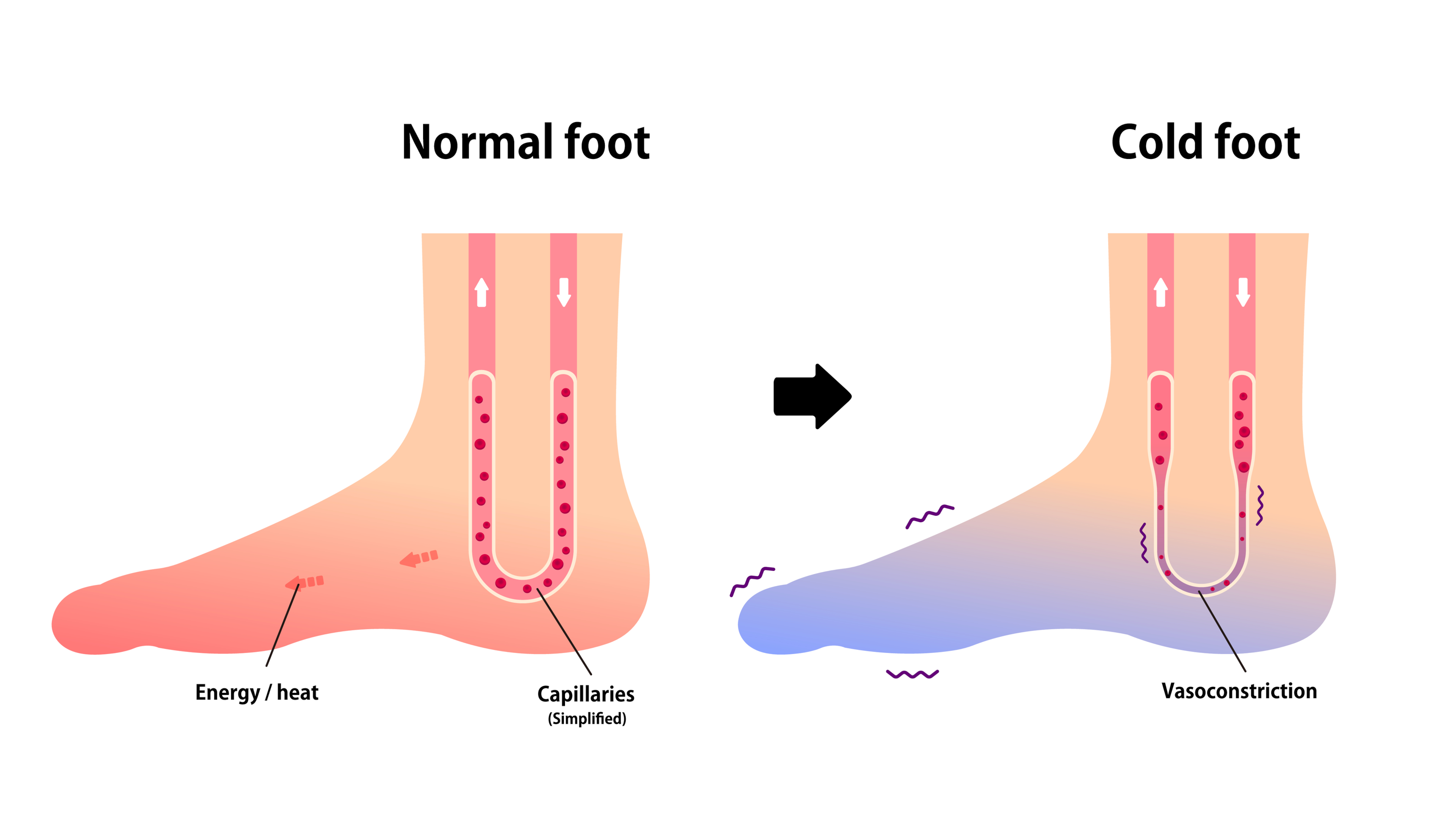
How Diabetes Affects Your Foot Temperature
Apart from causing pain, diabetes can also affect your foot temperature. This is because the nerve damage caused by diabetes can disrupt the normal functioning of the sweat glands in your feet, leading to dry and cracked skin. This dryness can further increase the risk of infection.
Moreover, diabetes can also impact the blood circulation in your feet, leading to a condition known as peripheral arterial disease (PAD). PAD can cause your feet to feel colder than the rest of your body due to insufficient blood flow. Therefore, monitoring your foot temperature regularly and consulting your healthcare provider if you notice any significant changes is essential.
Foot Problems Caused by Diabetes
Diabetes can cause a variety of foot problems. These include peripheral neuropathy, the most common and causes loss of feeling in the feet, and autonomic neuropathy, which affects the nerves that control the sweat glands, leading to dry and cracked skin.
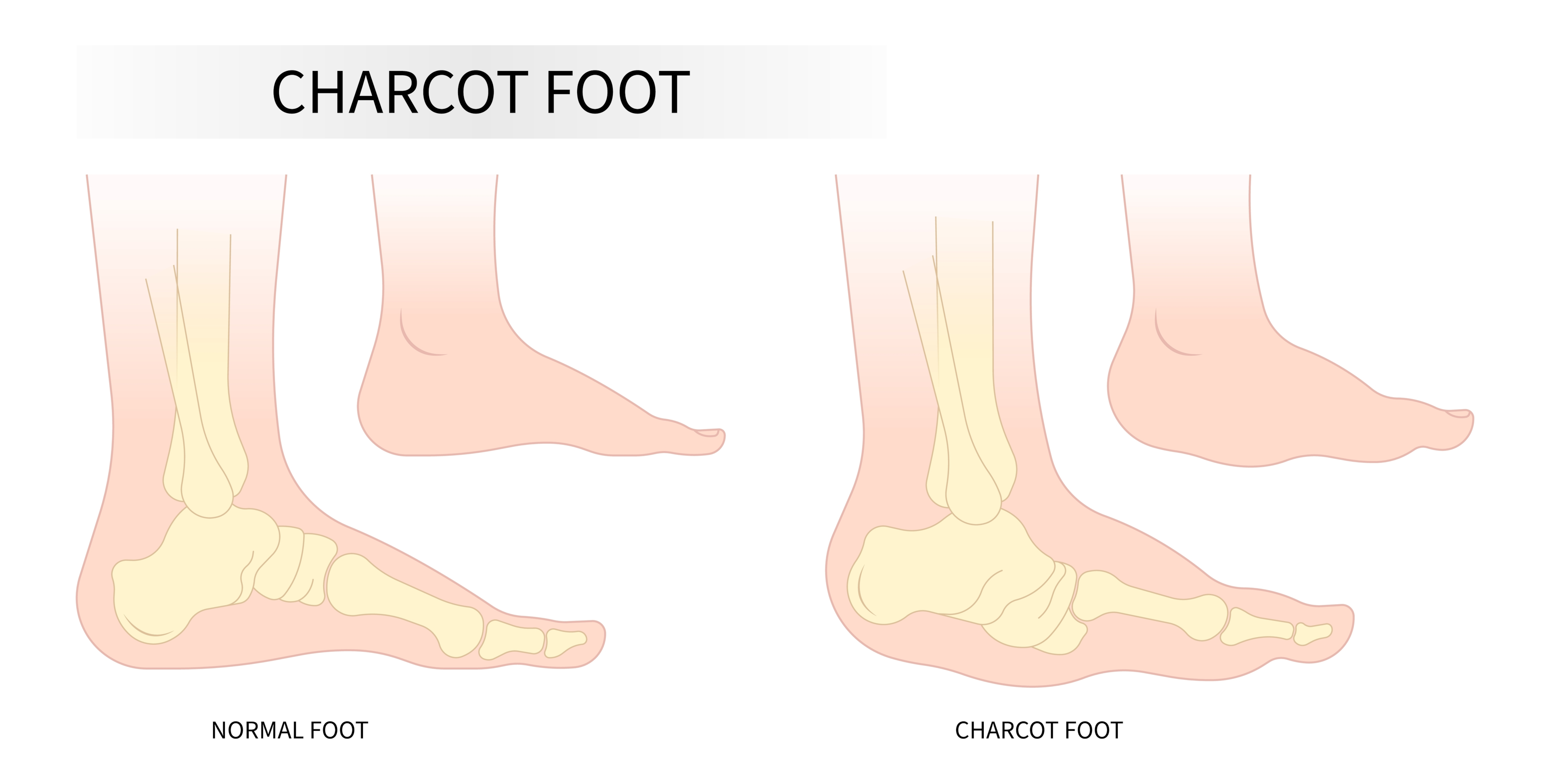
Another common problem is peripheral arterial disease, which reduces blood flow to the feet, making them vulnerable to infections and slow-healing wounds. Diabetes can also lead to structural changes in the feet, such as bunions, hammertoes, and Charcot foot, a serious diabetes complication.
How to Spot Diabetic Foot Infections Causing Foot Pain
Diabetic foot infections can be severe if not detected and treated promptly. Therefore, it’s crucial to know how to spot them. Some common signs of a foot infection may include redness, swelling, warmth, pain, and pus or drainage from a wound. You may also notice a foul smell or discoloration of the skin.
If you have numbness in your feet due to diabetic neuropathy, you may not feel pain or discomfort associated with an infection. Therefore, it’s important to visually inspect your feet daily for any signs of injury or infection. If you notice any of these symptoms, please feel free to seek medical help immediately.
Diabetic Neuropathy: Numbness and Tingling in Feet
One of the critical symptoms of diabetic neuropathy is numbness and tingling in the feet. This is due to the nerve damage that transmits sensations from the feet to the brain. The numbness can make it difficult to feel pain or temperature changes, increasing the risk of unnoticed injuries.
The tingling sensation, often described as pins and needles, can be uncomfortable and disruptive. It can also lead to losing balance and coordination, making walking or performing routine activities difficult. It’s essential to consult your healthcare provider if you experience persistent numbness or tingling in your feet.
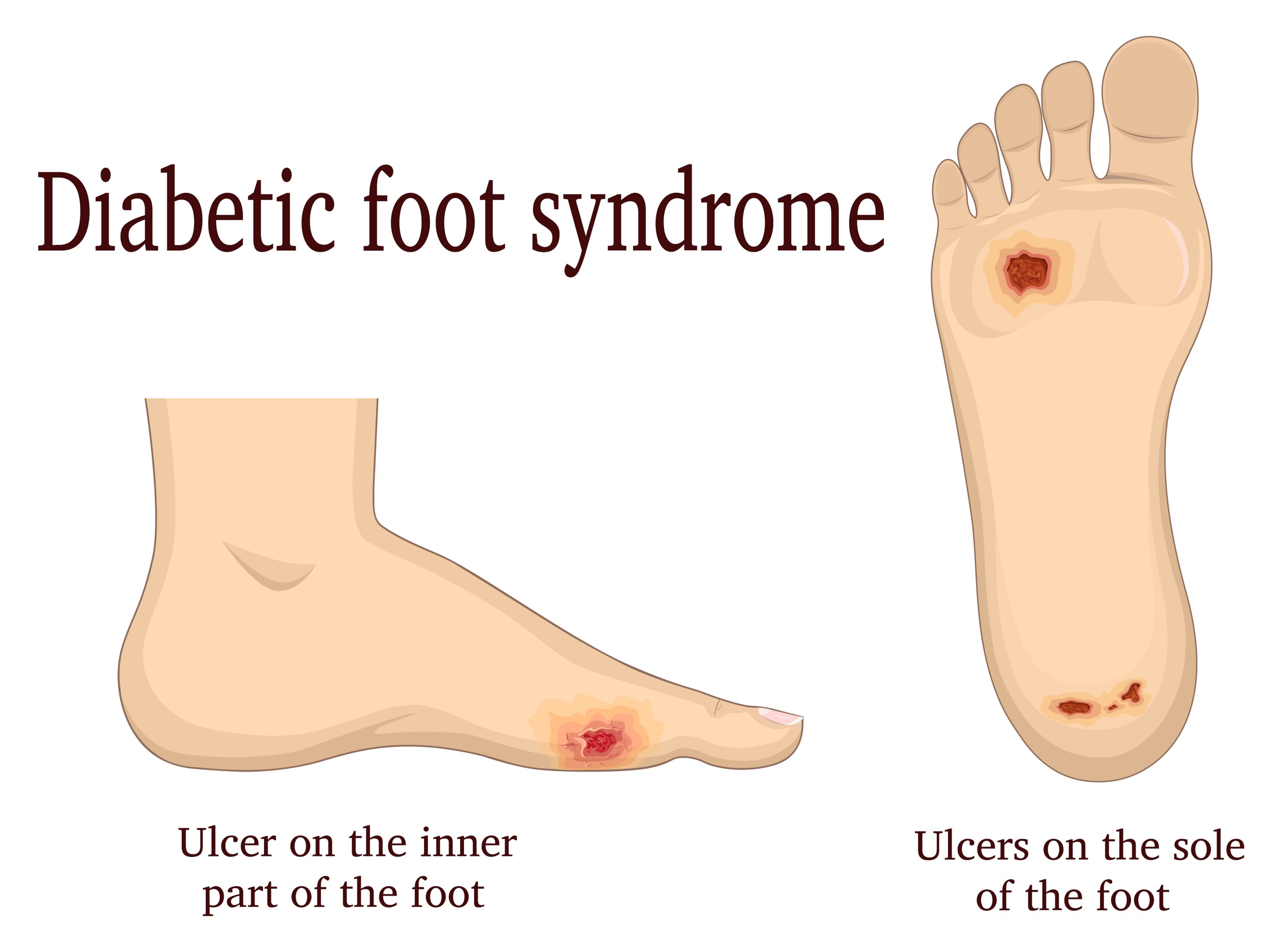
Diabetic Foot Ulcers: Prevention and Treatment
Diabetic foot ulcers are a common complication of diabetes and can lead to severe outcomes if not treated promptly. They often occur on the bottom of the foot and are caused by poor circulation, nerve damage, and pressure or friction from ill-fitting shoes and tight socks.
Preventing diabetic foot ulcers involves regular foot care, including daily inspection of the feet, keeping them clean and moisturized, and wearing comfortable shoes. If you notice any sores, blisters, or cuts on your feet, treat them immediately and consult your healthcare provider.
Treating diabetic foot ulcers involves cleaning and dressing the wound, controlling blood sugar levels, and sometimes, antibiotics or other medications. In severe cases, surgical intervention may be necessary to remove dead tissue or to relieve pressure on the ulcer.
Charcot Foot: A Serious Diabetes Complication
Charcot foot is a severe complication of diabetes, characterized by the weakening of the bones in the foot. Over time, this can lead to fractures and dislocations, causing the foot to become deformed. The condition often occurs in people with severe neuropathy who can’t feel pain or discomfort in their feet.
Recognizing the signs of Charcot’s foot is crucial for early intervention. These signs include redness, warmth, swelling, and changes in the foot’s shape. If you notice any of these symptoms, please feel free to seek medical help immediately. Treatment usually involves immobilizing the foot to allow the bones to heal and custom footwear to prevent further damage.
Diabetic Blisters: What to Do and Avoid
Diabetic blisters, also known as bullosis diabeticorum, are a rare complication of diabetes. They are similar to burn blisters and usually occur on the hands, feet, legs, and forearms. The exact cause of diabetic blisters is unknown, but they are more common in people with diabetic neuropathy.
If you have diabetic blisters, it’s important to avoid popping or puncturing them, as this can lead to infection. Instead, consult your healthcare provider, who may drain the blisters sterilely. Avoid tight shoes, use moisturizing creams to prevent blisters, and closely monitor your blood glucose levels.
Dry Skin and Cracks in Diabetic Feet
Dry skin and cracks are common in diabetic feet due to nerve damage affecting the sweat glands. These cracks can be painful and may bleed, increasing the risk of infection. Therefore, keeping your feet moisturized is essential to prevent dryness and cracking.
You can use a moisturizing cream or lotion to hydrate your skin, but avoid applying it between your toes, which can lead to fungal infections. Also, avoid soaking your feet for long periods, as this can strip the natural oils from your skin, causing further dryness. If you notice any severe cracks or bleeding, check your feet, and you can consult your healthcare provider.
Fungal Nail Infections in Diabetic Feet
Fungal nail infections, or onychomycosis, are common in people with diabetes. This is because the elevated blood sugar levels create an ideal fungus environment. These infections can cause the nails to become discolored, thick, and brittle and may lead to pain or discomfort.
To prevent fungal nail infections, keep your feet clean and dry, change your socks regularly, wear shoes, and avoid walking barefoot in public places like swimming pools or showers. If you notice any nail changes, consult your healthcare provider, who can prescribe antifungal medication.
Diabetic Foot Care: Tips and Best Practices for Foot Pain
Proper foot care is crucial for people with diabetes to prevent complications and maintain healthy feet. This involves daily inspection of the feet, washing them with warm water and mild soap, drying them thoroughly, especially between the toes, and moisturizing them to prevent dryness and cracking.
It’s also essential to wear comfortable shoes that fit well and provide good support. Avoid tight shoes or socks that can cause pressure or rubbing. Regularly trim your toenails to prevent ingrown nails or cuts. If you have difficulty caring for your feet due to neuropathy or other complications, seek the help of a podiatrist or healthcare professional.
Living With Diabetic Neuropathy and Diabetic Foot Pain
Living with diabetic neuropathy can be challenging, but with the proper knowledge and care, you can manage your symptoms and prevent further complications. Remember to monitor your symptoms closely, maintain a healthy lifestyle, and work closely with your healthcare provider.
Understanding the symptoms of diabetic foot pain and diabetic neuropathy is crucial to managing your condition effectively. Taking proactive steps towards foot care can significantly reduce your risk of complications and improve your quality of life. Remember, you are not alone in this journey; many resources and support are available to help you navigate it.
Video Credits: Doctor O’Donovan
Frequently Asked Questions on Diabetic Foot Pain in Relation to Diabetic Neuropathy
What is diabetic foot pain, and how does it relate to neuropathy?
Diabetic foot pain is a specific type of pain experienced by individuals with diabetes, often as a result of diabetic neuropathy. It can involve various sensations, including burning, stabbing, or aching pain in the feet.
When should I seek medical attention for diabetic foot pain or neuropathy?
To avoid serious complications, you should seek medical attention if you experience any new or worsening symptoms, such as foot ulcers, signs of infection, or severe pain. Regular check-ups with your doctors are also crucial for monitoring your condition.
What are some self-care tips for individuals with diabetic foot pain?
Self-care tips include inspecting your feet daily for cuts, sores, or signs of infection. Wear comfortable shoes and also wear warm socks. Also, keep your feet clean and dry, and avoid smoking and excessive alcohol consumption.
Discover Total Foot Comfort at Feet-Relief.com!
Are you tired of aching, tired feet? Seeking the ultimate relief for your hardworking soles? Look no further than Feet-Relief.com – your haven for all things foot comfort and wellness!
🦶 Step into Comfort: At Feet-Relief.com, we understand the importance of happy, pain-free feet. Our website is a treasure trove of solutions designed to pamper and rejuvenate your tired tootsies.
🌟 The Footwear Revolution: Explore our handpicked selection of innovative and orthopedically designed footwear. From cozy slippers to supportive insoles, our range is meticulously curated to provide the utmost comfort for every step you take.
🩺 Expert Advice: Worried about finding the perfect fit? Our team of foot experts is here to guide you. Get personalized recommendations and tips to keep your feet healthy and pain-free.
📚 Foot Care Knowledge Hub: Knowledge is power, and we empower you with a comprehensive resource hub. Dive into articles, guides, and tips on foot health, ensuring you make informed choices for your precious feet.
🛒 Easy Shopping: With a user-friendly interface and secure checkout, shopping for foot comfort has never been easier. We offer convenient shipping options to your doorstep, ensuring your comfort is just a click away.
🤝 Customer-Centric Experience: We take pride in our commitment to customer satisfaction. If you ever have questions, concerns, or need assistance, our friendly support team is just a message away.
🔐 Trust and Quality: At Feet-Relief.com, we prioritize quality and safety. All our products are sourced from reputable brands and undergo rigorous quality checks.
Say goodbye to foot discomfort and hello to blissful relief. Visit Feet-Relief.com today and take that first step towards healthier, happier feet. Your feet deserve the best, and we’re here to provide it.