BraceAbility Night Splint Sock Review: Ultimate Heel Pain Relief?
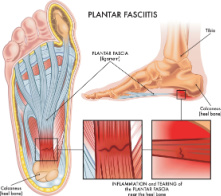
Dealing with plantar fasciitis or Achilles tendonitis can be a real nightmare, especially when it comes to finding a comfortable and effective solution for nighttime relief. We’ve recently tried the BraceAbility Plantar Fasciitis Night Splint Sock, and we believe it’s a game-changer for those suffering from heel pain.
The soft and flexible night splint sock is designed to provide a therapeutic stretch to your plantar fascia while you sleep. The adjustable strap pulls back on your toes, allowing the connective tissue to heal properly overnight. Not only does it alleviate heel pain, but it also offers support for issues like heel spurs and tendon arch pain.
Thoughtfully redesigned based on customer feedback, the updated version of this splint sock now features medical-grade materials, a wider toe box, a longer ankle strap for a secure fit, and a more effective toe stretching strap. Wearing the BraceAbility night splint sock is definitely more comfortable and less cumbersome than sleeping with a rigid plantar fasciitis boot.
Bottom Line
The BraceAbility Plantar Fasciitis Night Splint Sock is an excellent option for anyone seeking relief from plantar fasciitis, Achilles tendonitis, heel spurs, and other related discomforts.
Comfortable, low-profile, and effective, it’s worth trying out for a better night’s sleep and improved daytime mobility.
Don’t wait any longer. Click here to purchase the BraceAbility Plantar Fasciitis Night Splint Sock and experience the relief you deserve today!
Product Overview: BraceAbility Night Splint Sock
We recently tried the BraceAbility Night Splint Sock designed to alleviate heel pain and treat conditions like plantar fasciitis, Achilles tendonitis, and heel spurs. This soft, low-profile brace is specifically for nighttime use, offering support and a deep, therapeutic stretch to the plantar fascia while you sleep.
Initial impressions show the sock’s improvements with its medical-grade materials, wider toe box, longer ankle strap for a secure fit, and a more effective toe stretching strap, all based on valuable customer feedback. While getting used to sleeping with your foot in dorsiflexion might take some time, the splint sock is lightweight and less cumbersome than a rigid boot. Additionally, it can be worn on either your right or left foot.
The BraceAbility Night Splint Sock is designed for adults and comes in multiple sizes. To choose the appropriate size, reference the sizing chart provided in the product images. Overall, it’s an innovative solution for those who need relief from heel and foot pain associated with various conditions.
Custom Fit and Secure Design
Wearing the BraceAbility Plantar Fasciitis Night Splint Sock, we found comfort and relief through its customized fit and secure design. It’s suitable for both the right and left foot, offering an adjustable strap for a personalized, therapeutic stretch. The improved design now includes medical-grade materials and a wider toe box, ensuring a comfortable experience while wearing it overnight.
We noticed a significant difference in daytime mobility after consistently wearing this low-profile brace overnight. Unlike inserts and insoles, the consistent stretch from the night splint sock alleviates heel pain and supports healing for conditions like plantar fasciitis, Achilles tendonitis, and heel spurs.
While it takes some time to get used to sleeping with a foot in dorsiflexion, the lightweight construction and secure design make adaptation easier compared to a rigid plantar fasciitis boot. Overall, the BraceAbility Plantar Fasciitis Night Splint Sock provides a great balance of comfort, effectiveness, and usability for those seeking relief from foot and heel pain.

Alleviates Heel Pain
We found that the BraceAbility Plantar Fasciitis Night Splint Sock effectively alleviates heel pain over time. This sock is designed to address not only plantar fasciitis, but also Achilles tendonitis, heel spurs, and tendon arch pain. Unlike inserts and insoles that offer temporary relief, this night splint sock provides longer-lasting results.
The key to its effectiveness lies in wearing the sock while sleeping. It comes with an adjustable strap that pulls back on your toes, providing a deep, therapeutic stretch to your plantar fascia. This allows the connective tissue to heal properly overnight, creating noticeable improvements in daytime mobility.
Getting used to sleeping with your foot in dorsiflexion may take some time, but the low-profile design of this night splint sock is much more comfortable and easier to adapt to compared to rigid plantar fasciitis boots. The redesigned version, with medical-grade materials, a wider toe box, and a more effective toe stretching strap, accelerates the healing process even more.
Our experience with the BraceAbility Plantar Fasciitis Night Splint Sock has been positive in delivering relief from heel pain, without needing additional interventions or treatments.
Ideal for Nighttime Use
When it comes to finding relief for plantar fasciitis, Achilles tendonitis, heel spurs, and tendon arch pain, the BraceAbility Plantar Fasciitis Night Splint Sock excels, particularly for nighttime use. We tried this soft plantar fascia stretcher brace and found that wearing it during sleep significantly improved our daytime mobility.
The adjustable strap provides a deep, therapeutic stretch to the plantar fascia, allowing the connective tissue to heal properly overnight. No more relying solely on inserts and insoles for temporary relief!
Although it takes some time to get used to sleeping with your foot in dorsiflexion, the low-profile and lightweight design of this night splint sock made it much easier to adapt to than a rigid plantar fasciitis boot. The updated design (as of March 2019) features medical-grade materials, a wider toe box, a longer ankle strap for a secure fit, and a more effective toe stretching strap to accelerate the healing process.
In our experience, this BraceAbility compression sleeve truly shines as a nighttime solution for heel pain relief.
Lightweight and Low-Profile Brace
We’ve found the BraceAbility Plantar Fasciitis Night Splint Sock to be a game-changer for those suffering from foot and heel pain. It’s lightweight and low-profile, making it much easier to get used to than a rigid plantar fasciitis boot. The updated design, as of March 2019, features medical-grade materials, a wider toe box, and a more effective toe stretching strap to speed up the healing process.
This splint sock is intended for nighttime use, promoting better mobility during the day. The adjustable strap delivers a deep, therapeutic stretch to the plantar fascia while you sleep, allowing the connective tissue to heal properly overnight. Alleviating pain from plantar fasciitis, Achilles tendonitis, heel spurs, and tendon arch pain, this brace offers a long-term solution compared to temporary relief from inserts and insoles.
The BraceAbility splint sock can be worn on either the right or left foot, and finding the right size is easy with the aid of their sizing chart. Overall, the lightweight and low-profile brace provides a comfortable and effective alternative for plantar fasciitis therapy.
Pros and Cons
We found the BraceAbility Plantar Fasciitis Night Splint Sock to effectively alleviate heel pain by providing a deep, therapeutic stretch to the plantar fascia. Customers reported experiencing relief from conditions such as plantar fasciitis, Achilles tendonitis, heel spurs, and tendon arch pain after consistent use.
The low-profile brace design is lightweight and more comfortable than a rigid plantar fasciitis boot, making it easier to get used to for nighttime use. Its adjustable strap allows for a secure fit, and it can be worn on your right or left foot. The wider toe box, longer ankle strap, and medical-grade materials are recent improvements based on customer feedback, showing that BraceAbility is responsive to their customers’ needs.
Despite its overall effectiveness, some users mentioned a few drawbacks. The splint is somewhat uncomfortable and can be quite hot during sleep, especially for those without air conditioning. There’s also an issue with the grippy material on the bottom of the sock that makes it difficult to move around in bed.
The Velcro attachment’s length seems inadequate, potentially limiting the range of motion for those with larger feet or requiring more tension. Some users also reported that the brace did not provide enough of a stretch to their feet when lying down.
In summary, the BraceAbility Plantar Fasciitis Night Splint Sock is a potentially effective solution for those looking to alleviate heel pain and improve mobility. However, some users may find it uncomfortable or lacking in specific features, ultimately affecting its overall efficacy.
Customer Reviews
We’ve had the opportunity to use the BraceAbility Plantar Fasciitis Night Splint Sock and explore the experiences of many customers using this product. With a 3.7-star rating from 4,176 users, it has been a popular choice amongst people looking for relief from plantar fasciitis and Achilles tendonitis-related discomfort.
Many customers expressed relief from the pain and discomfort caused by plantar fasciitis thanks to this night splint sock. Some found the product helpful in combination with other treatments but mentioned that it could be uncomfortable. A useful tip shared by one user was to cut a rounded piece of cardboard and stuff it into the sock for added comfort.
A few users didn’t find the product effective in giving the required stretch needed for relieving plantar fasciitis. On the other hand, some appreciated the build and functionality of the product, stating that it already helped them.
The splint sock was considered too hot for users without air conditioning, and some had difficulty adjusting the Velcro attachment for the desired stretch. Despite this, many customers still found the BraceAbility Plantar Fasciitis Night Splint Sock worth trying out and appreciated the relief it provided them.
Conclusion
In our experience, the BraceAbility Plantar Fasciitis Night Splint Sock has its pros and cons. On the positive side, it does provide relief from plantar fasciitis pain, as it helps stretch the foot and Achilles tendon during sleep. It is also well-made, and many users have reported improvements in their condition after using it.
However, there are a few downsides we have noticed. Some users find the sock uncomfortable to wear and claim it doesn’t pull the foot up enough for optimal relief. Other users mention that the sock can be quite hot, especially without air conditioning, and the grippy material at the bottom may make moving around in bed difficult.
While the BraceAbility sock might not be perfect for everyone, it has certainly helped many people through their plantar fasciitis journey. We recommend giving it a try if you are looking for a simple and supportive solution to alleviate heel pain but be prepared to adjust to the possible discomforts mentioned above. Ultimately, it comes down to individual preferences and needs.
Frequently Asked Questions
How effective are night splints for treating plantar fasciitis?
Night splints, like the BraceAbility Plantar Fasciitis Night Splint Sock, can effectively treat plantar fasciitis. Many users have reported improvements in their heel pain and mobility. The adjustable toe strap provides a deep, therapeutic stretch to the plantar fascia. This allows the connective tissue to heal properly as you sleep. However, it is important to note that individual results may vary. Treatment effectiveness also depends on consistency in wearing the splint. Combining it with other treatments like proper footwear and exercises helps, too.
What is the recommended duration for wearing a night splint?
It is generally recommended to wear the BraceAbility Plantar Fasciitis Night Splint Sock while sleeping, around 6 to 8 hours per night. It may take some time to get used to wearing the splint, but consistency is key in relieving plantar fasciitis pain. Please consult your healthcare provider to determine the optimal duration based on your specific condition and needs.
How to properly wear a night splint for best results?
To wear the BraceAbility Plantar Fasciitis Night Splint Sock correctly, follow these steps:
- Put the splint sock on your affected foot, ensuring it covers your heel and ankle comfortably.
- Adjust the ankle strap, ensuring it is snug but not too tight.
- Secure the toe strap by pulling it back, providing a deep stretch to your plantar fascia while keeping your toes comfortable.
- Adjust the straps as needed for a secure fit.
Ensure that the splint sock is not overly tight or uncomfortable, as it may interfere with your sleep or cause additional discomfort.
Are compression socks beneficial for plantar fasciitis?
Yes, wearing compression socks can be beneficial for those with plantar fasciitis. They help improve blood circulation, reduce inflammation, and provide support to the plantar fascia. While the BraceAbility Plantar Fasciitis Night Splint Sock is not specifically a compression sock, the combination of a night splint and compression socks can be an effective treatment strategy for dealing with plantar fasciitis pain.
Are plantar fasciitis braces suitable for walking?
The BraceAbility Plantar Fasciitis Night Splint Sock is designed primarily for nighttime use and may not be suitable for walking or regular daily activities. While some customers may find it comfortable enough to walk in for short periods, it is advised to focus on using the splint sock during sleep for maximum therapeutic benefits. For walking support, consider using specialized footwear, orthotic inserts, or a daytime brace specifically designed for plantar fasciitis support during daily activities.