Plantar Fasciitis Activity Modifications: Smart Adjustments for Daily Life
Plantar Fasciitis Activity Modifications: Smart Adjustments for Daily Life
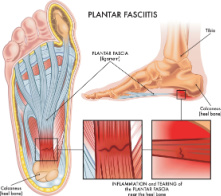
Plantar fasciitis is a common cause of heel pain, affecting millions of people globally. The condition occurs when the plantar fascia, a band of tissue that connects the heel bone to the toes, becomes inflamed or degenerated. This inflammation can result in sharp, stabbing pain in the heel or the bottom of the foot, especially during the first steps in the morning or after periods of inactivity. Various factors, such as the type of shoes, foot structure, overuse, and walking surfaces, can contribute to the development of plantar fasciitis.
To manage plantar fasciitis effectively, a combination of treatments, including activity modifications, is often recommended. These modifications aim to reduce stress on the plantar fascia and promote healing without completely stopping physical activity. By adjusting one’s exercise routine, choosing proper footwear, and incorporating stretching and strengthening exercises, individuals can alleviate symptoms and prevent future occurrences of plantar fasciitis.
Key Takeaways
- Plantar fasciitis is a common cause of heel pain resulting from inflammation or degeneration of the plantar fascia.
- Activity modifications, such as adjusting exercise routines and choosing the correct footwear, can help manage and prevent plantar fasciitis.
- Incorporating stretching and strengthening exercises into one’s daily routine can alleviate symptoms and promote healing.

Understanding Plantar Fasciitis
What is Plantar Fasciitis
Plantar fasciitis is a common foot condition caused by inflammation of the plantar fascia, a thick band of tissue connecting the heel bone to the toes. This fascia helps support the arch of the foot and plays a vital role in walking and other foot movements. When the plantar fascia becomes inflamed, it leads to heel pain and stiffness, which can interfere with daily activities.
Symptoms of Plantar Fasciitis
The primary symptom of plantar fasciitis is heel pain. Individuals may experience a sharp, stabbing pain at the bottom of the heel, often most noticeable in the mornings or after long periods of rest. The pain typically worsens with increased activity and may also extend to the arch of the foot. As the condition progresses, stiffness in the toes and a limited range of motion become more apparent.
Diagnosis of Plantar Fasciitis
To diagnose plantar fasciitis, a healthcare professional will conduct a physical exam to assess the area of pain and evaluate the patient’s foot mechanics. In some cases, imaging tests such as X-rays or MRIs may be necessary to rule out other potential causes or to identify any associated conditions like heel spurs.
Causes and Risk Factors
Plantar fasciitis can result from various factors, including age, stress on the feet, and poor foot mechanics. Some common risk factors include:
- Age: The risk of developing plantar fasciitis increases with age, especially for individuals between the ages of 40 and 60.
- Obesity: Being overweight or obese can put additional stress on the plantar fascia, contributing to inflammation and pain.
- Activity: Runners and individuals frequently exercising on hard surfaces are more susceptible to developing plantar fasciitis.
- Foot Mechanics: Having a high arch or flat feet can affect the distribution of weight on the foot, leading to increased stress on the plantar fascia.
- Tightness: Tightness in the calf muscles or Achilles tendon can cause increased strain on the plantar fascia.
By understanding plantar fasciitis, its symptoms, diagnosis, and risk factors, individuals can take necessary measures to manage the condition and minimize its impact on their daily activities. In some cases, simple activity modifications, such as wearing appropriate footwear or using athletic tape for support, can help alleviate pain and promote healing.

Activity Modifications for Plantar Fasciitis
Modifying Exercise and Movement
When dealing with plantar fasciitis, it is crucial to adjust and modify exercises to alleviate pain and prevent further damage. Opt for low-impact exercises such as swimming, cycling, or yoga to lessen the strain on your feet. It is advisable to avoid high-impact activities such as running, jumping, and extended periods of standing or walking.
Incorporate daily stretching exercises that target the calf muscles and plantar fascia to improve flexibility and diminish pain. Remember to gradually increase the intensity of your exercises while closely monitoring your pain levels.
Footwear Adjustments
The type of shoes you wear plays a significant role in managing plantar fasciitis. Opt for shoes with proper arch support and cushioning. You can also use shoe inserts or orthotics to provide extra support and reduce stress on your plantar fascia. Heel cups can also be added to improve shock absorption.
Avoid walking barefoot and limit wearing unsupportive footwear, as it can exacerbate the symptoms. Replace worn-out shoes regularly to maintain proper foot support.
Lifestyle Changes
Implementing certain lifestyle changes can also help mitigate the symptoms of plantar fasciitis. Ensure you are giving your feet adequate rest and elevating them when possible to reduce inflammation.
Applying ice to the affected area several times a day can help alleviate pain and inflammation. You can also try icing while rolling your foot over a frozen water bottle for additional relief.
Managing your weight is crucial, as excessive weight can increase pressure on your plantar fascia. Establishing a balanced diet and participating in low-impact exercises can help maintain a healthy weight.
By incorporating these activity modifications, you can effectively manage plantar fasciitis symptoms and prevent further damage to your feet.

Treatment Options for Plantar Fasciitis
Non-Surgical Treatments
Plantar fasciitis is usually treated with non-surgical methods aimed at relieving heel pain and inflammation. These conservative treatments include medications, shoe modifications, physical therapy, and lifestyle changes.
Anti-inflammatory medications such as non-steroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation and alleviate pain. Examples of NSAIDs include ibuprofen, naproxen, and aspirin.
Shoe modifications involve using supportive shoes and custom orthotics, like heel cups and arch supports, to reduce the strain on the plantar fascia.
Physical therapy plays an essential role in treating plantar fasciitis. Exercises and stretches designed to strengthen the plantar fascia, Achilles tendon, and lower leg muscles are beneficial sources. A trained therapist may also teach proper athletic taping techniques to support the foot.
Night splints are used to help stretch the plantar fascia and Achilles tendon overnight, maintaining a gentle tension to promote a healing source.
Ice massage can help to reduce inflammation and ease pain. Applying ice to the affected area for 15-20 minutes a few times a day is helpful in managing symptoms.
Surgical and Advanced Treatments
If conservative treatments do not provide relief after a few months, more advanced options may be explored.
Steroid injections can be administered to reduce inflammation and provide temporary pain relief. However, repeated injections can weaken the plantar fascia over time and are not recommended as a long-term solution.
Platelet-rich plasma (PRP) injections involve using the patient’s own blood enriched with platelets to promote healing in the affected area. Some studies have shown PRP to be as effective or more effective than steroid injections in treating plantar fasciitis source.
Extracorporeal shock wave therapy (ESWT) uses high-energy shock waves to stimulate healing in the plantar fascia. While some patients may experience pain relief after ESWT, it is not always a guarantee and more research is needed to determine its overall effectiveness source.
Laser therapy applies low-level laser energy to reduce inflammation and stimulate the healing process. It is a non-invasive option with minimal side effects and can be considered as an alternative to more invasive treatments.
Surgery for plantar fasciitis is generally considered a last resort, reserved for patients who have not found relief with other treatments. The surgical procedure involves releasing part of the plantar fascia, but it carries the risk of complications and may not guarantee complete pain relief.

Dealing with Chronic Plantar Fasciitis
Long-Term Management Strategies
Chronic plantar fasciitis can be managed with a combination of activity modifications, stretching exercises, and other conservative treatment approaches. One of the primary treatment strategies involves stretching the plantar fascia, calf muscles, and Achilles tendon. Strengthening exercises targeting the calf muscles and foot arch can provide additional support to the plantar fascia and reduce the risk of recurring pain.
Custom orthotics can also help alleviate heel pain by providing proper support to the arch of the foot and redistributing pressure evenly across the plantar surface. Over-the-counter insoles may be effective for some, while others might require prescription orthotics designed specifically for their individual needs. It’s important to note that nonoperative treatments, including activity modification, anti-inflammatory medication, gastrocnemius and plantar fascia stretching, and in-shoe orthosis, can lead to complete resolution of pain in 90% of patients, but may take 3-6 months.
Coping with Persistent Heel Pain
For those coping with persistent heel pain due to chronic plantar fasciitis, it’s essential to consider other treatment options. Night splints can help maintain a gentle stretch to the plantar fascia and Achilles tendon overnight, reducing morning stiffness and discomfort. In cases where a heel spur is present, heel cups or pads can provide extra cushioning and help to relieve pressure.
Degeneration of the connective tissue in the plantar fascia may lead to chronic heel pain. Pain management strategies, such as ice or heat application, over-the-counter pain relievers, and corticosteroid injections, can offer temporary relief. Additionally, anti-inflammatory medications can reduce inflammation and alleviate pain in the short term.
It is crucial to maintain a consistent routine of stretching exercises as it plays a vital role in long-term management. Gastrocnemius and plantar fascia stretches can help prevent muscle contracture and improve flexibility. Establishing a balance between activity modification and strength training is essential to prevent exacerbating symptoms while still promoting muscle strengthening. Remember to consult with a healthcare professional before starting any new exercise regimen.

Conclusion
Incorporating activity modifications can significantly improve the recovery process for individuals suffering from plantar fasciitis and heel pain. By following a consistent regimen of appropriate exercises and stretching, as well as implementing recommended orthotic devices, patients can experience relief from pain in 90 percent of cases within 3 to 6 months.
It is essential for individuals to focus on both muscle strengthening and stretching to effectively address the root causes of plantar fasciitis. Techniques such as ice massage, activity modification, and anti-inflammatory medications can also play a critical role in addressing the condition and promoting healing, as recommended by the AAFP.
It is crucial to understand that plantar fasciitis recovery may take time, and patience is necessary for success. The condition affects both sedentary and athletic individuals and may result from chronic overload, either due to lifestyle or exercise factors. Therefore, addressing the condition requires a comprehensive and consistent approach.
In conclusion, plantar fasciitis activity modifications can be highly effective in managing heel pain and promoting recovery. By combining these modifications with targeted exercises, stretches, and other recommended treatments, individuals can expect to experience significant improvements in their condition. However, it is essential to maintain patience and persistence throughout the healing process, as recovery may take several months. Following a knowledgeable and clear plan, most individuals can overcome plantar fasciitis and enjoy a pain-free lifestyle.
Frequently Asked Questions
What exercises are safe with plantar fasciitis?
It is crucial to choose exercises that do not place undue strain on the plantar fascia while healing. Low-impact activities such as swimming, cycling, and yoga can be safe choices for individuals with plantar fasciitis. Additionally, implementing specific stretches and exercises targeting the plantar fascia and surrounding muscles may aid in recovery and pain reduction.
How can I modify my workout routine to avoid aggravating plantar fasciitis?
To prevent aggravation of plantar fasciitis, focus on low-impact activities and gradually build intensity as your condition improves. Be cautious with high-impact sports, such as running, and instead opt for alternatives like brisk walking or using a treadmill with proper shock absorption. Remember to wear well-cushioned shoes that support your arches and consider using inserts or orthotics if necessary.
Which activities should I avoid if I have plantar fasciitis?
Activities that involve repetitive impacts on the feet, like running, jumping, or plyometrics, can exacerbate plantar fasciitis symptoms. High-intensity sports, such as basketball and tennis, may also worsen the condition due to rapid changes in direction and pressure on the plantar fascia. Avoid these activities during the healing phase and reintroduce them cautiously as you recover.
What are the best stretches to alleviate plantar fasciitis pain?
Stretches targeting the plantar fascia, Achilles tendon, and calf muscles can help alleviate pain and improve flexibility. Incorporate exercises such as the plantar fascia stretch, calf stretch, and towel or band-assisted stretches into your daily routine. Consult a healthcare professional or physical therapist for personalized recommendations and proper stretch guidelines.
How can I tell if my plantar fasciitis is healing?
Signs of plantar fasciitis healing include a gradual reduction in pain levels, especially in the morning or after prolonged rest, and improved flexibility in the foot and ankle. It is essential to monitor your symptoms and consult with your healthcare provider regularly to assess progress and ensure proper treatment.
How can I speed up the healing process for plantar fasciitis?
Accelerating the healing process for plantar fasciitis includes taking a multifaceted approach. This may involve rest, proper footwear or orthotics, exercises specifically targeting the plantar fascia and surrounding muscles, and incorporating anti-inflammatory measures such as ice or over-the-counter medications. A healthcare professional can help determine the most suitable treatment plan for your situation.