Fungal Nail Infections in Diabetic Feet: An In-depth Analysis
Living with diabetes is akin to navigating a daily labyrinth of health challenges, where vigilance and discipline are your guiding stars. Among the many hurdles, one often-overlooked concern that silently plagues those with diabetes is the issue of fungal nail infections in diabetic feet. This seemingly innocuous condition holds the potential to unleash a cascade of complications, all stemming from the intricate interplay between high blood sugar levels and your body’s ability to heal itself. In this exploration, we delve into the world of fungal nail infections, or onychomycosis, in diabetic individuals. Discover the profound connection between diabetes and toenail fungus, the lurking risk factors, the subtle symptoms, and the importance of timely diagnosis and care. Join us on this journey to ensure that you’re well-equipped to safeguard your feet – the unsung heroes of your daily life – against this often underestimated threat.
Photo by Engin_Akyurt on Pixabay
Fungal Nail Infections in Diabetic Feet
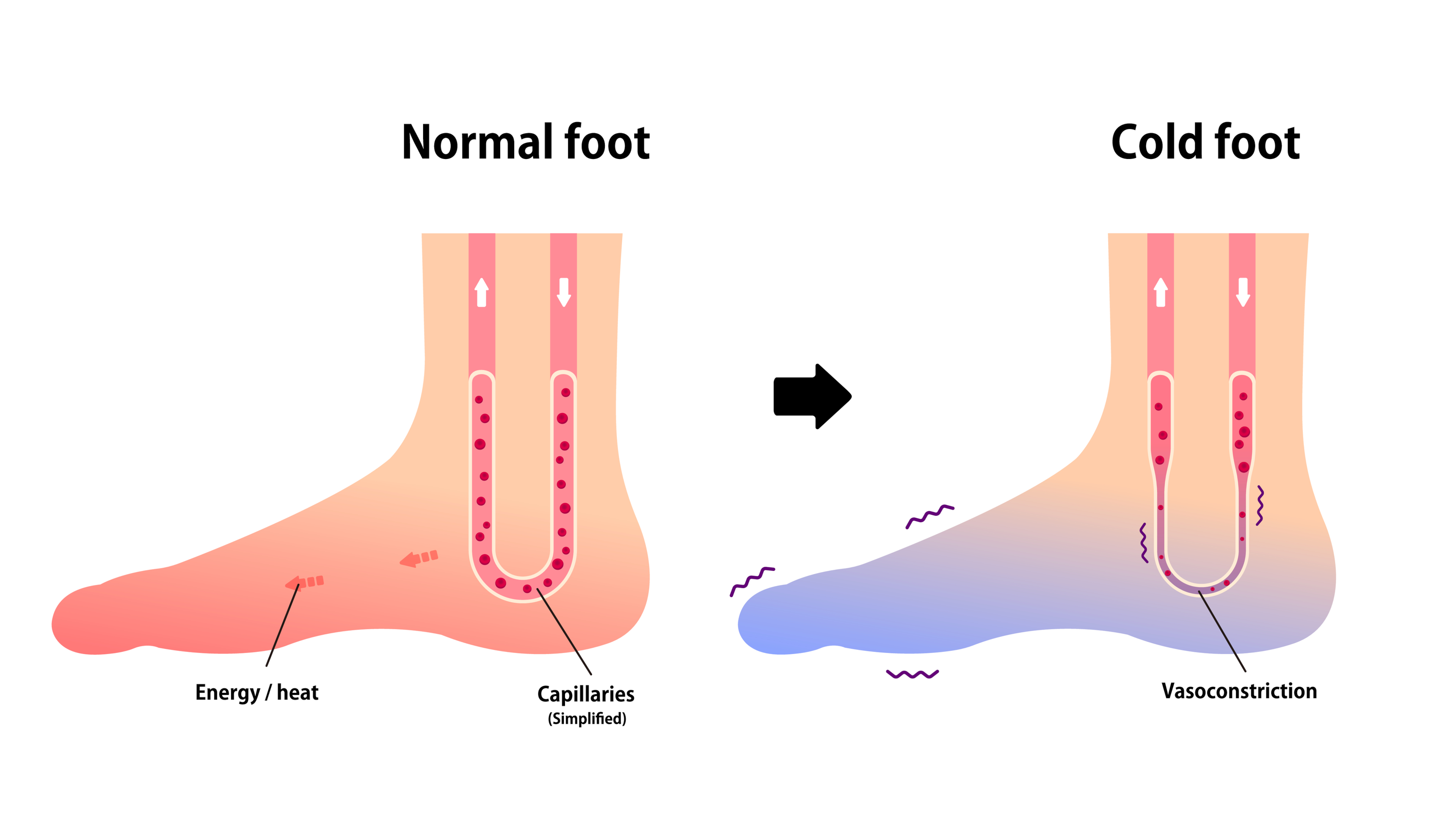
Living with diabetes is a constant challenge, and managing it requires diligence and discipline. One of the most common complications associated with diabetes is foot problems specifically fungal nail infections. A diabetic foot is susceptible to various infections and other complications due to the high blood sugar levels that compromise the body’s natural healing process. The condition reduces blood flow to the feet, with poor circulation and making it harder for wounds, sores, and infections to heal.
Furthermore, nerve damage, also known as diabetic neuropathy, is another common complication of diabetes. It can cause numbness in the feet, making a person unaware of any sores, blisters, or injuries that may have occurred. It is crucial to understand the various types of diabetic foot problems, including fungal nail infections in diabetic feet, to manage them effectively.
Among the numerous foot-related issues that diabetics face, fungal nail infections are quite prevalent. These infections are not only unsightly but can also lead to severe complications if left untreated. Therefore, understanding these infections is paramount to ensure proper foot care in diabetics.
Understanding Fungal Nail Infections
Fungal nail infections, medically known as onychomycosis, are common infections of the toenails or fingernails that result from the overgrowth of fungi in, under, or on the nail. Fungi thrive in warm, moist environments, making shoes a perfect breeding ground. The infection begins as a white or yellow spot under the nail polish and can cause the nail to discolor, thicken, and crumble at the edge as it progresses. It can affect several nails but usually not all of them.
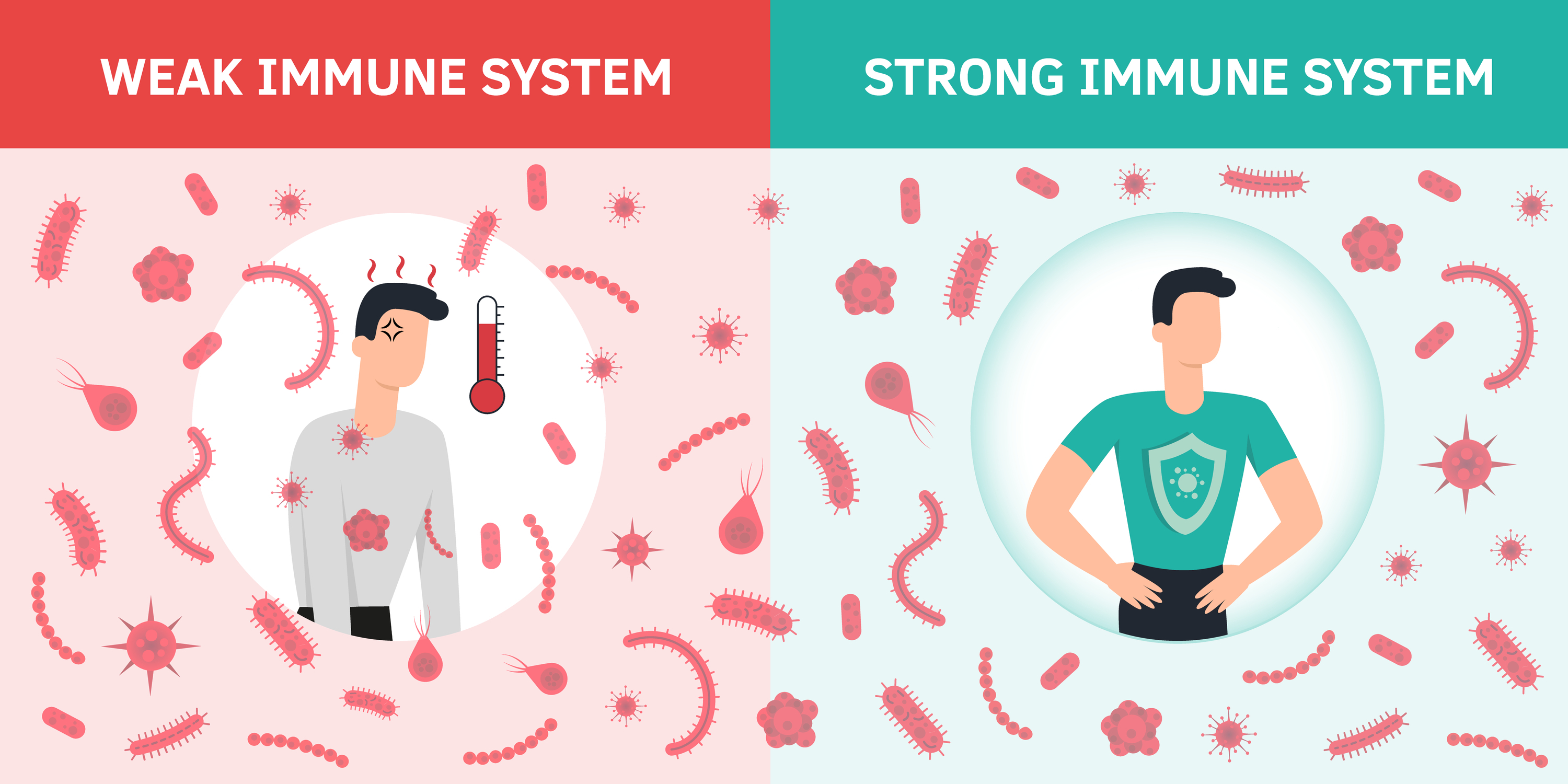
While anyone can develop a fungal nail infection, certain factors increase the risk. These include aging, having a weakened immune system, and living with conditions such as diabetes. A nail injury or skin condition, like psoriasis, can also make someone more susceptible to getting a fungal nail infection.
Moreover, fungal nail infections are notoriously difficult to treat, and they can recur even after successful treatment. Also, they can lead to more serious complications, such as cellulitis (a skin infection) or other secondary infections, especially in people with weakened immune systems or diabetes.
The Connection: Diabetes and Toenail Fungus
There is a strong correlation between diabetes and nail fungus. Diabetics are more susceptible to fungal nail infections due to the impairment of their immune system. High blood glucose levels can weaken the immune system, making it less able to fight off infections. This susceptibility to secondary bacterial infections is the reason why diabetics often struggle with recurrent infections.
Moreover, the nerve damage caused by diabetes can lead to a loss of sensation in the feet, a condition known as diabetic neuropathy. It means a diabetic person may not notice a fungal infection in its early stages, allowing it to progress and become more challenging to treat.
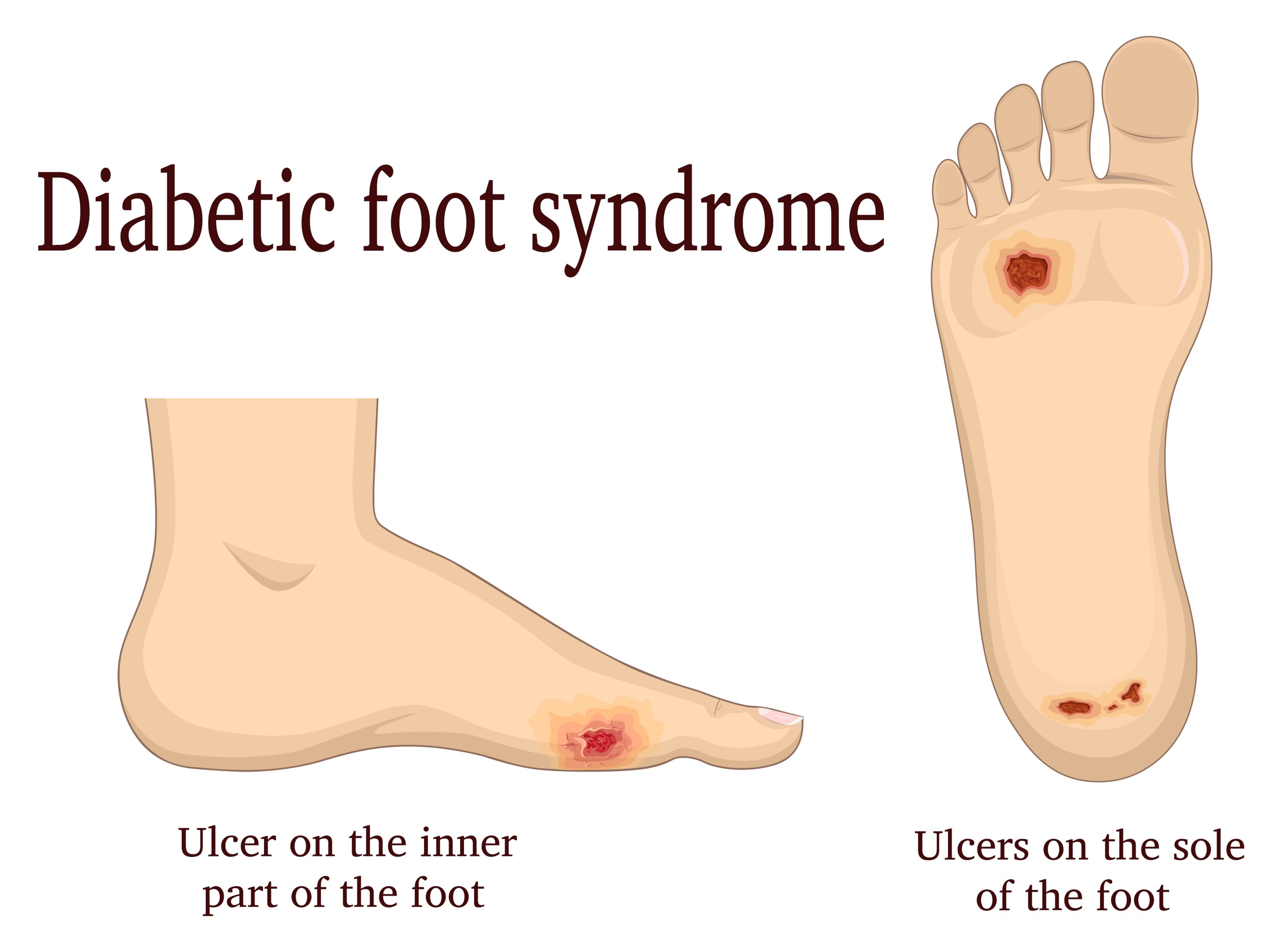
As such, fungal nail infections in diabetic feet are not merely cosmetic problems. They can have serious implications, leading to painful sores and even contributing to the risk of foot ulcers. Therefore, understanding the connection between diabetes and toenail fungus is essential for managing and preventing these infections.
What Causes Toenail Fungus in Diabetics?
Several factors contribute to the development of toenail fungus in diabetics. High blood sugar levels, which are a hallmark of diabetes, create an environment conducive to fungal growth. Moreover, the reduced blood flow to the feet, another common complication of diabetes, denies the feet the nutrients and oxygen necessary to fight off infections.
In addition, the nerve damage caused by diabetes often leads to dry skin on the feet. This dryness can cause small cracks in the skin, providing an entry point for fungi. Footwear that is too tight or doesn’t allow the feet to breathe can also promote fungal growth.
Furthermore, a history of athlete’s foot or nail injuries, or the use of communal showers or swimming pools, can increase the risk of developing a fungal nail infection. It is important to understand these risk factors to effectively prevent and manage toenail fungus in diabetes.
Video Credit: @AADskin
How Does Diabetes Cause Toenail Fungus?
Diabetes does not directly cause toenail fungus; however, it creates conditions conducive for fungal growth, leading to infections. High blood glucose levels can suppress the immune system and lower the body’s resistance to infections, including fungal infections.
Moreover, poor blood circulation in the feet, a common problem in diabetics, means that the body’s natural defense mechanisms can’t reach the site of the infection effectively. This problem allows the infection to take hold and thrive.
In addition, nerve damage caused by diabetes can lead to numbness in the feet. As a result, a person with diabetes may not notice the early signs of a fungal infection, such as a discolored toenail, until the infection has progressed.
Symptoms of Fungal Nail Infections in Diabetic Feet
Symptoms of fungal nail infections in diabetic feet can be subtle in the early stages. They often start with a small white or yellow spot under the nail. As the infection progresses, the nail may become discolored, thickened, and brittle, often crumbling at the edges.
In some cases, the infected nail can separate from the nail bed, a condition known as onycholysis. This separation can cause discomfort and pain. Sometimes, a foul odor may be present, and the nail plate surrounding skin may also become inflamed or scaly.
In severe cases, a fungal nail infection can cause significant pain and discomfort, making it difficult to walk or wear shoes. If the infection spreads to the skin, it can lead to cellulitis, a serious skin infection that requires immediate medical attention.
Diagnosing Fungal Nail Infections in Diabetics
Diagnosing fungal nail infections in diabetics involves a thorough examination of the affected nails and a review of the diabetic patient’s medical history. The doctor may take a small sample of the nail or the debris under it to examine under a microscope or to culture in a lab. This examination can help identify the type of fungus causing the infection and guide the appropriate treatment.
It’s important to note that other conditions, such as psoriasis, dermatitis, and certain nail injuries, can mimic the symptoms of a fungal nail infection. Therefore, a correct diagnosis is crucial to ensure effective treatment.
Moreover, regular check-ups are essential for people with diabetes. These check-ups can help detect fungal nail infections in their early stages, making treatment more successful and preventing potential complications.
Treatment Options for Diabetic Toenail Fungus
There are several treatment options available for diabetic toenail fungus. The choice of treatment largely depends on the severity of the infection and the diabetic patient population’s overall health.
Topical antifungal medications, such as creams, ointments, and nail lacquers, are commonly used to treat mild to moderate infections. These medications are applied directly to the infected nail and surrounding skin.
For more severe infections, oral antifungal medications may be prescribed. These medications are more effective than topical treatments as they attack the infection from within. However, they can have side effects and may interact with other medications, so they should be used under the supervision of a healthcare provider.
In some cases, surgical treatment may be necessary. The infected nail may need to be removed to allow a new, healthy nail to grow back. Laser therapy is another option, which uses light to kill the fungus.
It’s important to note that treatment of fungal nail infections can be a slow process as nails grow slowly. It can take several months to a year for the nail to clear up completely.
Prevention Tips: Avoiding Toenail Fungus with Diabetes
Preventing toenail fungus with diabetes involves maintaining good foot hygiene and controlling blood sugar levels. Here are some steps you can take to prevent fungal nail infections:
- Wash your feet daily with soap and water and dry them thoroughly, especially between the toes.
- Wear breathable shoes and socks that wick away moisture.
- Avoid walking barefoot in communal areas such as swimming pools and showers.
- Regularly inspect your feet for any signs of infection, such as discolored nails or skin cracks.
- Keep your toenails trimmed straight across and file down thickened areas.
- Regularly disinfect your nail clippers and files.
- Control your blood sugar levels to boost your immune system and make your body less hospitable to fungi.
Remember, prevention is better than cure. A little care can go a long way in preventing fungal nail infections in your diabetic patients’ feet.
The Role of Regular Foot Care in Diabetes
Regular foot care plays a crucial role in managing diabetes. Given the complications associated with diabetes, including fungal nail infections, it’s essential to take good care of your feet.
Regular foot inspections can help detect any problems early before they become serious. Look for any cuts, sores, or changes in the nails, such as discoloration or thickening. If you notice any changes, seek medical attention promptly.
Foot hygiene is equally important. Washing your feet daily and keeping them dry can prevent fungal infections. Additionally, moisturizing your feet can prevent dry skin and cracks that can become entry points for fungi.
Finally, wearing the right footwear can prevent foot injuries and keep your feet dry, reducing the risk of fungal infections. Choose shoes that fit well and allow your feet to breathe. Also, change your socks regularly to keep your feet dry.
Fungal Nail Infection: Summary
In conclusion, fungal nail infections in diabetic feet are a common complication that can lead to serious problems if left untreated. Understanding the connection between diabetes and toenail fungus, knowing what causes toenail fungus in diabetics, and recognizing the symptoms can help in managing these infections effectively.
Treatment options for diabetic toenail fungus are available, but prevention through good foot care and blood sugar control is the best approach. Remember, your feet carry you through life. Taking good care of them is an essential part of managing diabetes.
And finally, if you suspect you have a fungal nail infection, seek medical advice promptly. Early detection and treatment can prevent complications and improve your overall quality of life.
FAQs Fungal Nail Infections
When should a diabetic person see a healthcare provider for a fungal nail infection?
Diabetic individuals should consult their healthcare provider as soon as they suspect a fungal nail infection. Early treatment and monitoring are crucial to prevent complications.
How is a fungal nail infection diagnosed in diabetics?
A healthcare provider can diagnose a fungal nail infection by checking the affected nails and may perform a nail scraping or culture to confirm the presence of fungi.
How can diabetic individuals prevent fungal nail infections?
To prevent fungal nail infections, diabetics should:
- Keep their feet clean and dry.
- Trim nails straight across and not too short.
- Wear thin shoes and socks.
- Avoid walking barefoot in public places like locker rooms.
- Be cautious when getting pedicures and ensure the salon maintains good hygiene practices.
Step into a World of Foot Care Excellence: Discover Feet-Relief.com!
For more in-depth guidance and resources on managing diabetes-related foot issues, we invite you to explore the wealth of information available at Feet-Relief.com.
At Feet-Relief.com, we understand that your feet are your daily companions on life’s journey, and their well-being is paramount. Our comprehensive website is a dedicated hub for all things related to foot care, particularly in the context of diabetes.
Why Feet-Relief.com?
- Expert Insights: Our platform is curated by a team of experienced researchers who link with professionals specializing in diabetic foot care. You’ll find articles, guides, and resources that are grounded in medical expertise and the latest research.
- Comprehensive Information: Whether you’re seeking advice on managing toenail fungus, preventing foot ulcers, or understanding the nuances of diabetic neuropathy, Feet-Relief.com offers comprehensive information to empower you with knowledge.
- Lifestyle Tips: We recognize that managing diabetes isn’t just about medical treatment—it’s a lifestyle. Discover practical tips on choosing the right footwear, maintaining proper hygiene, and controlling blood sugar levels.
- Community Support: Connect with others who share similar experiences and challenges through our online community. Share stories, exchange advice, and find the support you need.
- Regular Updates: Our team is dedicated to keeping you informed with the latest developments in diabetic foot care. Subscribe to our newsletter to receive regular updates and insights delivered directly to your inbox.
At Feet-Relief.com, we believe that well-informed individuals are better equipped to navigate the complexities of diabetes and its associated foot issues. Our mission is to empower you with the knowledge and resources you need to ensure your feet remain healthy, allowing you to lead a fulfilling life with diabetes.
Visit Feet-Relief.com today and embark on a journey towards better foot health. Your feet deserve nothing less.