FIT KING EMS Foot Massagers Review
FIT KING EMS Foot Massagers Review: Is It Worth Your Money?
When it comes to managing foot discomfort, finding relief is often a top priority. I recently had the chance to try out the FIT KING EMS Foot Massager, and it’s designed to alleviate a variety of foot-related ailments. Whether you’re suffering from neuropathy, plantar fasciitis, or simply the day-to-day aches that come with an active lifestyle, this device aims to provide some much-needed comfort.
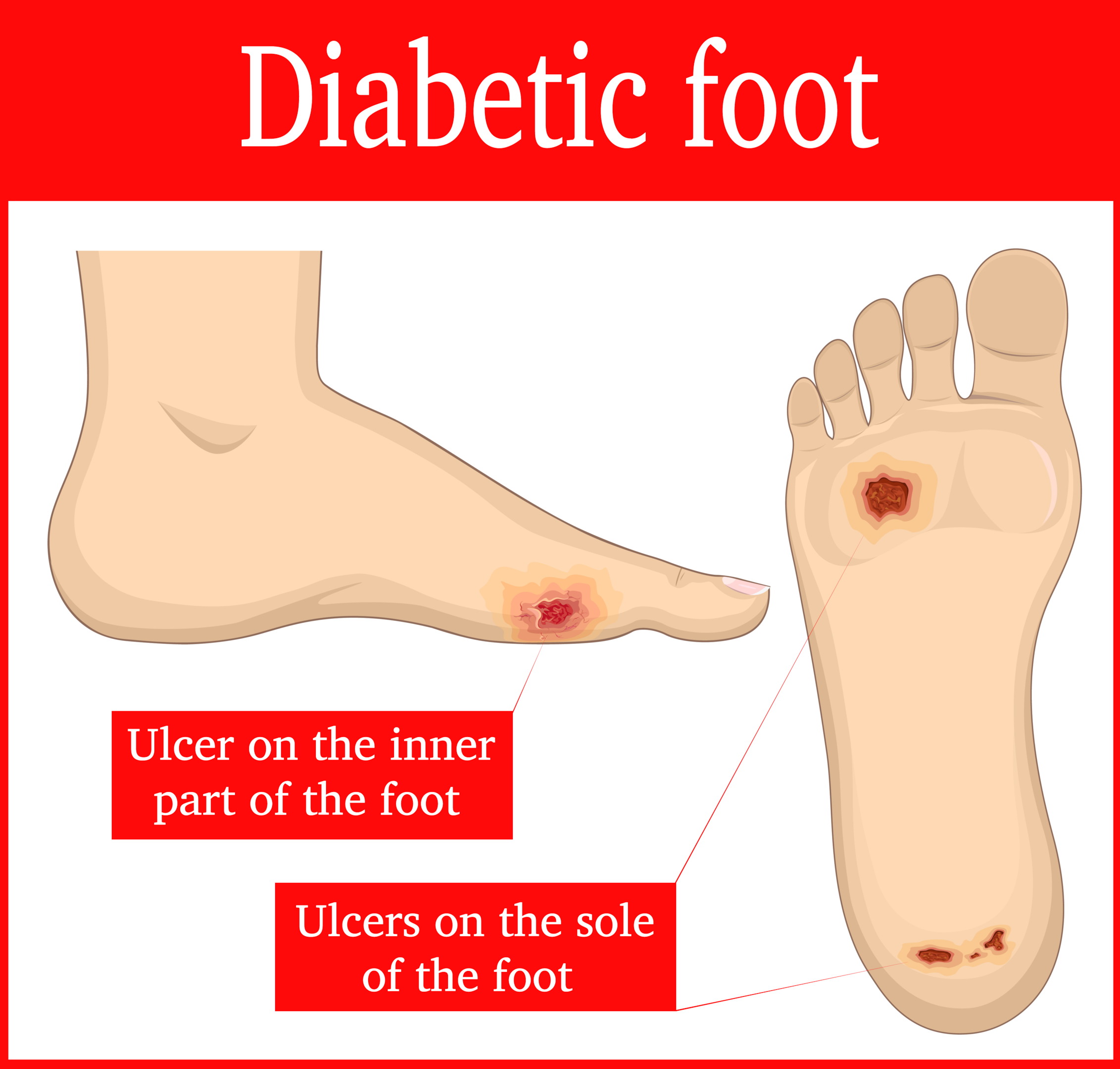
The unit combines EMS and TENS technologies, which are typically found in physical therapy settings to relax muscles and nerves and reduce swelling. Particularly intriguing is its claim to aid in pain relief from conditions like diabetes and arthritis. I found the usage to be straightforward, with a remote control that eliminates the need to bend over – a feature that many will appreciate.
Notably, the device is quiet in operation, which allows for relaxation without the added noise that some massagers produce. It offers a range of 10 modes and 99 intensity levels, so you can fine-tune your experience. For those who need more than just foot stimulation, the addition of TENS pads to target other body areas is a valuable bonus.
Bottom Line
The FIT KING EMS Foot Massager stands out for its multipurpose design and ease of use. If you’ve been struggling with foot or leg pain, this FDA-cleared medical device could be a game-changer in your daily routine.
By embracing technology typically seen in professional therapy, now available in the comfort of your home, you might just find the pain relief you’ve been searching for.
Interested in giving your feet the attention they deserve? Take a closer look at the FIT KING EMS Foot Massager and consider making it part of your wellness regimen.
Overview of FIT KING EMS Foot Massagers for Neuropathy
Imagine unwinding after a long day with a device that not only eases foot discomfort but also targets neuropathy and plantar fasciitis. The FIT KING EMS foot massager is an FDA Cleared Class II Medical Device that does just that, using EMS & TENS technology to relieve pain and improve circulation in your feet. You can enjoy a quiet session without any size restrictions or disturbing vibrations, thanks to the remote control that makes adjustments a breeze, especially for those who may have difficulty bending over.
While some users have described instant relief from leg tension and improved circulation, others have not found the expected pain relief, even at higher intensity levels. With a diverse range of features including 10 modes, 99 intensity levels, and additional TENS pads for body pain, the massager aims to cater to various needs. However, it’s important to start at a lower intensity and gradually find the level that feels right for you.
Your satisfaction is backed by a customer-friendly return policy and dedicated support, although it’s worth noting that usage is restricted for those under 18 or with certain medical conditions. While the product promises a comprehensive relief experience, your personal results may vary depending on individual sensitivity and health conditions.
Relief of Pain and Discomfort
When you’re grappling with neuropathy or plantar fasciitis, finding relief can feel like a never-ending quest. The FIT KING EMS Foot Massager aims to provide that respite through a combination of EMS and TENS technology. Users have reported that regular use, specifically around half an hour daily over a period of several weeks, significantly eases the discomfort associated with these conditions.
While it’s not a miracle cure, the convenience of the massager is undeniable – it’s silent, adaptable to any foot size, and the remote control means you won’t have to struggle with bending down to change settings. The massager’s principle is to use pads and a roller to stimulate and relax the muscles, which can be particularly helpful if you suffer from swollen feet or leg pain after long hours of standing or sitting.
Despite its straightforward utility, it might not be a one-size-fits-all solution. Some users with larger foot sizes have found the massager less effective, specifically in reaching the heel area. Moreover, a handful of comments have mentioned that the intensity, even when at its highest setting, was insufficient for their needs.
Remember, it’s vital to ensure this device is right for you, especially if you have medical conditions such as heart disease or are pregnant, as the device is not recommended in these cases. If you’re seeking a non-invasive aid to manage foot and leg pain, the FIT KING Massager may be worth considering, though it’s essential to manage expectations and understand that relief levels can vary from person to person.
Medical Device Certification
In considering the FIT KING foot massager, it’s reassuring to note its eligibility for FSA and HSA. This suggests a level of trust in the safety and efficacy of the device for health-related use. When a product is marked as FSA/HSA eligible, it typically means that it conforms to certain health and safety regulations and is deemed suitable for medical-related expenses. However, it’s crucial to understand that this mark of approval does not equate to FDA approval, which is a certification that requires more rigorous testing and compliance to specific medical device standards.
The presence of such certifications can provide a layer of confidence in the safety of the product you’re considering. It’s wise to keep in mind that while certifications indicate compliance with industry standards, individual experiences with the massager might vary. Always consider how the device feels during use; the gentle stimulation it offers should be soothing, yet effective for conditions like neuropathy and plantar fasciitis. Also, remember to consult with a healthcare professional, especially for conditions that require medical attention.
Versatile Pain Management
Experiencing pain in your legs and feet can be debilitating, but the FIT KING EMS Foot Massager offers a promising solution. Its primary function is to ease discomfort associated with conditions like neuropathy, plantar fasciitis, and arthritis. In your quest for relief, you’ll find the device’s combination of EMS and TENS therapies quite beneficial. These high-tech features target stiff muscles and nerves, potentially reducing swelling and enhancing circulation.
Managing different types of pain is made simple with the included body pads, addressing areas the foot unit can’t, like your back or arms. As your feet rest on the massager, you might enjoy the kneading action of the unique rollers, aimed at reducing muscle tightness. The quiet operation is a bonus, ensuring your relaxation sessions remain uninterrupted.
The device’s ease of use is notable, tailored to include those who may not be as tech-savvy. With a remote control, adjustments are straightforward, allowing you to change settings without bending over—ideal for users with limited mobility. Despite its benefits, the massager may not be perfect for everyone. It’s reported that the remote can be less effective for some, and individuals with larger feet may find the heel massage out of reach. Still, many find that it offers substantial relief where other products have fallen short. Proceed with confidence, as the FDA-approved material and comprehensive customer service indicate a commitment to your satisfaction and safety.
Ease of Use Features
When your feet ache after a long day, simplicity can be the ultimate relief. That’s what the FIT KING EMS Foot Massager delivers. With its remote control, adjusting settings is hassle-free, saving you from the strain of bending over. There’s no need to worry about fitting your feet into the device—it accommodates any size comfortably and operates without distracting noises or vibrations.
You’ll find 10 different modes and 99 intensity levels at your fingertips. For someone unfamiliar with EMS and TENS technology, these options allow you to start off gently and gradually find the strength that soothes your pains best. Starting around intensity level 20, most users sense the therapeutic pulses kicking in.
One of the handy features is the roller, adding to the versatility by offering a kneading function that eases plantar fasciitis symptoms. It’s designed to simplify your relaxation routine at home. However, remember that this device comes with precautions, so make sure to review them thoroughly before use, especially if you have certain health conditions. With a 30-Day Return and Exchange policy, you have the support you need should any issue arise.
Warranty and Safety Information
When it comes to your peace of mind, the FIT KING Foot Massager has you covered with a comprehensive warranty. Your investment is protected from the date of purchase, allowing you to relax even more while you use the device. The built-in safety features ensure that your experience with the massager is not only effective but also maintains the highest safety standards with its use of a corded electric power source.
Should you encounter any issues, customer service is responsive and the brand, known for its dedication to quality and user experience, stands behind their product. Remember to retain your proof of purchase, as this will be necessary if you need to make a claim. Safety-wise, the product is built from sturdy plastic materials and designed with your well-being in mind. Embrace the soothing relief with an assurance that you’re in good hands with FIT KING’s commitment to your satisfaction and safety.
Pros and Cons
Pros
Having used the FIT KING EMS Foot Massager, it’s time to discuss what makes it stand out. Your tense legs stand a good chance of relaxation, thanks to this device. It’s not just a matter of easing the muscles; the unit’s kneading functionality, combined with rotating balls, targets your circulation effectively.
This FDA Cleared Class II Medical Device employs EMS and TENS technology, indicating its safety and efficacy. If you have varying pain points, the inclusion of four TENS pads allows you to address discomfort beyond your feet, including areas like the calf, knees, and even your neck.
You’ll appreciate the ease of use. With a remote control, you can adjust modes without bending over, an excellent feature for elderly users. The array of 10 modes and 99 intensity levels presents a level of customization that puts you in control to find your optimal setting comfortably.
Some users have reported noticeable improvements in conditions like lymphedema, noting changes in leg and foot circulation within days of use.
Cons
However, it’s not without its flaws. If you’re a person with large feet, the massager might not suit you best – some users with size 11.5 feet and above have found the massager’s heel area to be ineffective.
Taking a critical look at the user interface, the remote control might not be as helpful as one would expect, leading to potential frustration.
The massager also doesn’t offer any heat function, which could be a letdown if warmth during massage is important for your relaxation.
Lastly, there’s mention of the massager reaching intense levels without delivering the expected sensations. This might indicate variability in experience or a challenge for those with a high threshold for stimulation. A few users have felt compelled to return the product as it did not meet their expectations for pain relief.
Customer Reviews
Having personally experienced the soothing effect of the FIT KING EMS Foot Massager, I can say it holds up to some of the praise it receives. Your tired legs might experience relief as you indulge in its kneading capabilities, and the rolling spheres can be a game-changer for your circulation. Many users enjoy the convenience of shiatsu massages right at home, appreciating the simple controls, and the ability to set massage durations according to their comfort.
While it brings a smile to many faces, the massager is not without its drawbacks. If your feet are on the larger side, like a size 11.5 or above, you might find the heel massage less accessible, which can be a deal-breaker if that’s your sore spot. Remote functionality has also come into question, with some finding it less beneficial.
For those seeking relief from conditions such as lymphedema, feedback suggests significant improvement in circulation with consistent use. However, some have reached maximum intensity without feeling the expected relief or the warming sensation, leading to disappointment. It’s clear the FIT KING EMS Foot Massager isn’t a one-size-fits-all solution, but for the right fit, it can be a spot of comfort in your daily routine.
Conclusion
After personally testing the FIT KING EMS Foot Massager, it’s clear that it offers a meaningful respite for those with sore legs and aching feet. Its effectiveness in alleviating symptoms of neuropathy and plantar fasciitis is noteworthy, particularly with its adjustable intensity and massage settings, which you can tailor to suit your comfort level. However, if you have larger feet, you might find this massager less accommodating, as it seems to cater to those with smaller foot sizes. Remote operations could be smoother, but this isn’t a deal-breaker given the primary function of the massager which does deliver relief.
The massager is quite user-friendly with a simple control interface, and the inclusion of an LCD screen makes it easy to monitor your settings. Though the foot massager is not without its flaws, such as lukewarm heating capabilities and limited reach for larger foot sizes, its customization options and overall performance make it a worthy consideration, especially for those seeking daily relief from foot discomfort. Overall, it represents a solid choice among home foot massager options.
Frequently Asked Questions
When it comes to the world of foot massagers, certain queries always seem to surface. Having recently put these devices through their paces, I’ve compiled answers to some of the most frequent questions, drawing from both personal experience and diligent research. Here’s what potential buyers like you might want to know.
What are the benefits of using an EMS foot massager for neuropathy?
EMS foot massagers are designed specifically to address issues like neuropathy. They massage your feet using electrical muscle stimulation (EMS), which can lead to a few key benefits:
- Alleviation of pain associated with neuropathy
- Increased circulation in the feet and legs
- Reduction in swelling and cramping
- Improvement in overall foot health
Consistent use might just make a noticeable difference in how your feet feel, especially if you’re dealing with nerve pain.
How do you operate a FIT KING leg massager with heat?
Operating a FIT KING leg massager is quite straightforward:
- Place your feet onto the massager.
- Power on the device using the remote control.
- Select your desired mode and intensity level.
- If your model has a heat function, choose the setting for warmth.
- Sit back and let the massager run through its program—typically about 30 minutes.
No bending over is necessary, which is a boon if you struggle with mobility.
Are EMS foot massagers effective according to medical professionals?
Many medical professionals acknowledge the potential benefits of EMS foot massagers for certain conditions. These devices are often FDA-cleared and are recognized to:
- Stimulate muscles and nerves beneficially
- Contribute to pain management strategies
- Support circulation issues
However, it is always recommended to consult with a healthcare provider to ensure it complements your individual medical needs.
Can you provide instructions for using an EMS foot massager?
Here are some simple instructions:
- Ensure the device is connected to power.
- Sit comfortably and rest your feet on the device.
- Turn on the massager and use the remote to choose a mode.
- Gradually adjust the intensity to your comfort level.
- Enjoy the session and turn the device off once completed.
Remember, starting at lower intensity levels and working your way up is key to a comfortable experience.
What is the recommended duration for a session with an EMS foot massager?
Typically, a single session should last around 20-30 minutes. Most devices will have preset timers for convenience. Continuous daily sessions over several weeks can provide optimal results, but it’s crucial to listen to your body and take breaks if needed.
What should one consider when comparing the FIT KING EMS foot massager to the Ryoku model?
When comparing any EMS foot massagers, like the FIT KING and Ryoku models, consider these factors:
- Intensity levels available to cater to different pain thresholds
- Ease of use, particularly if the massager will be used by someone with mobility issues
- Additional features, such as heated massage or TENS for pain relief
- Size and fit, especially if you have larger feet
It’s also sensible to glance through user reviews for personal testimonials regarding efficacy and comfort.
Read More
How Home Foot Massagers Improve Circulation and Boost Health