Cloud Massage Shiatsu Foot Massager Review: Is it Worth the Investment?
Looking for a foot massager that can relieve pain and improve circulation? We recently tried out the Cloud Massage Shiatsu Foot Massager and were impressed with its performance.
This machine is designed to provide relaxation and relief for a range of foot conditions, including plantar fasciitis and neuropathy. The heat therapy function is a bonus, providing soothing warmth to help ease tension and discomfort.
One of the standout features of the Cloud Massage Shiatsu Foot Massager is its deep kneading massage nodes, which work to target specific pressure points in the feet. The adjustable intensity settings allow you to customize your massage experience, ensuring maximum comfort and effectiveness.
We also appreciate the sleek and compact design of this foot massager, which makes it easy to store when not in use. And with its FSA/HSA eligibility, you may be able to use your health savings account to purchase it.
Bottom Line
Overall, we highly recommend the Cloud Massage Shiatsu Foot Massager for anyone looking to improve their foot health and relieve pain. Its powerful massage nodes, heat therapy function, and adjustable intensity settings make it a top choice for at-home foot massage therapy. So why wait? Click here to purchase the Cloud Massage Shiatsu Foot Massager and start enjoying the benefits today!
Cloud Massage Shiatsu Foot Massager Overview
We recently had the opportunity to try out the Cloud Massage Shiatsu Foot Massager, and we were quite impressed with its features. The adjustable bar allows for a deep kneading shiatsu massage at the optimum comfort angle, unlike other foot massagers that force you to keep your knees together and legs at a 90-degree angle.
The dual massage feature provides multiple settings for heat, air compression pressure, and vibration, making it perfect for your feet, calves, toes, and ankles. The foot/calf area is 5″ wide and open-toed, 11″ long with air pressure cuffs deflated.
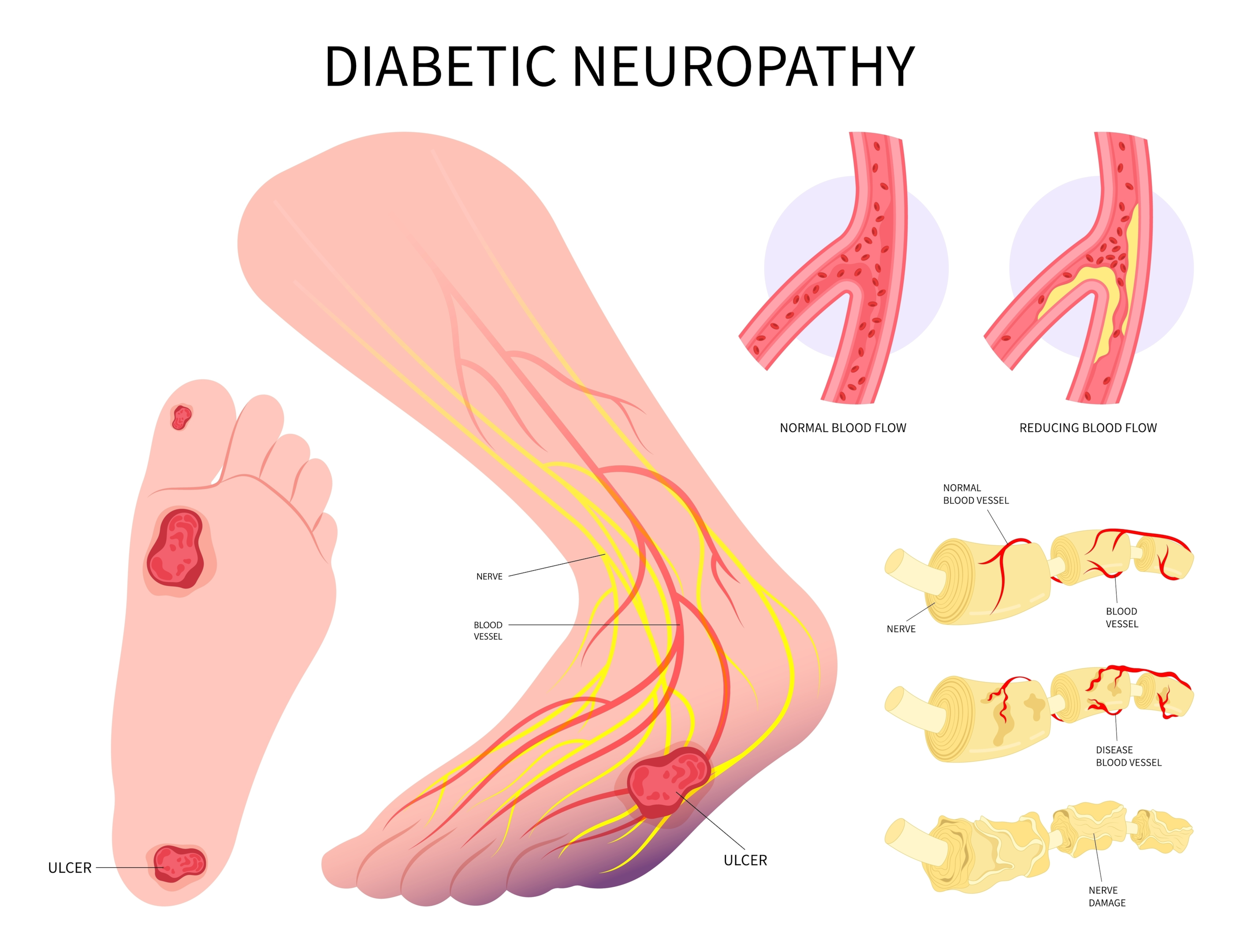
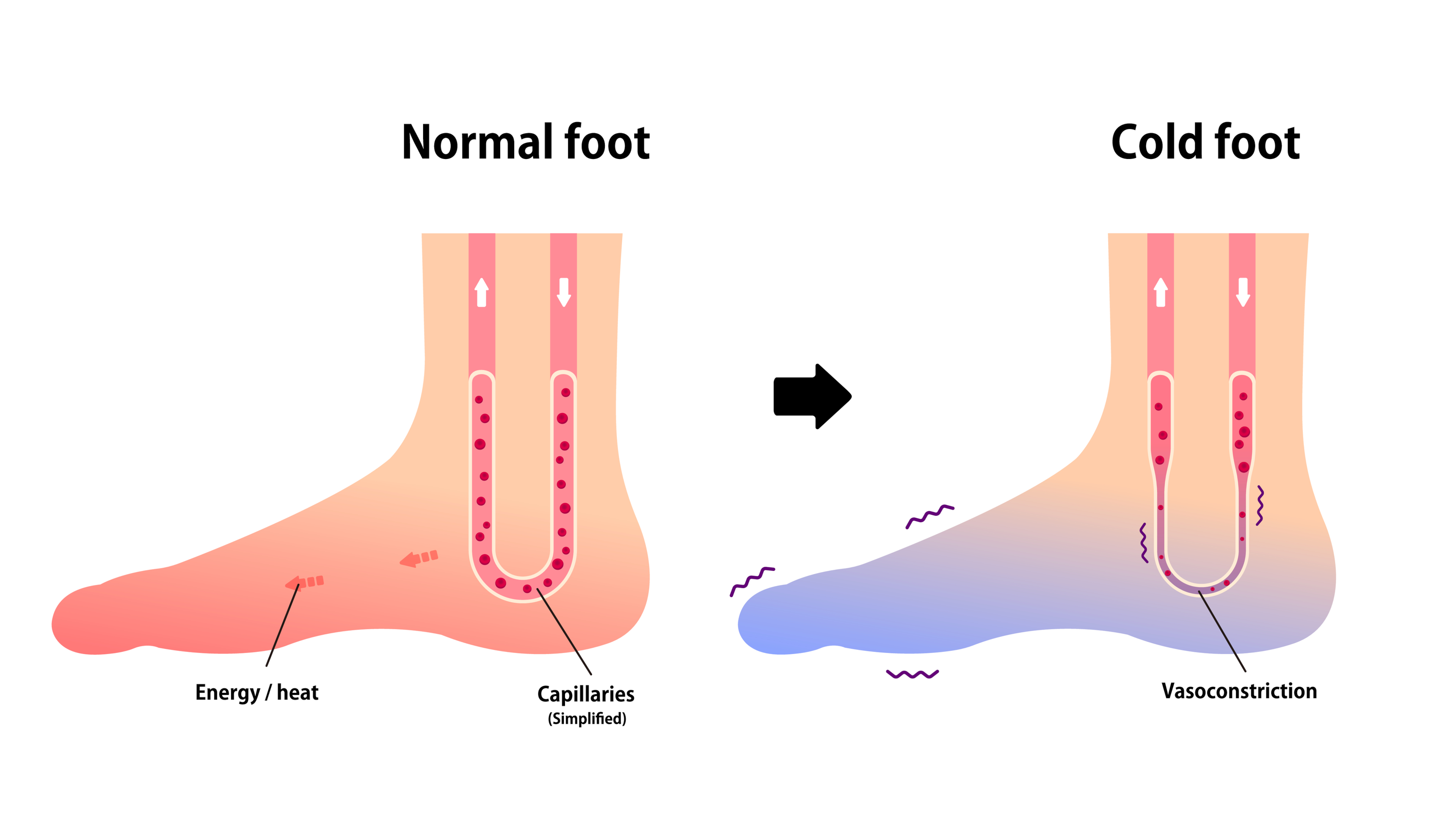
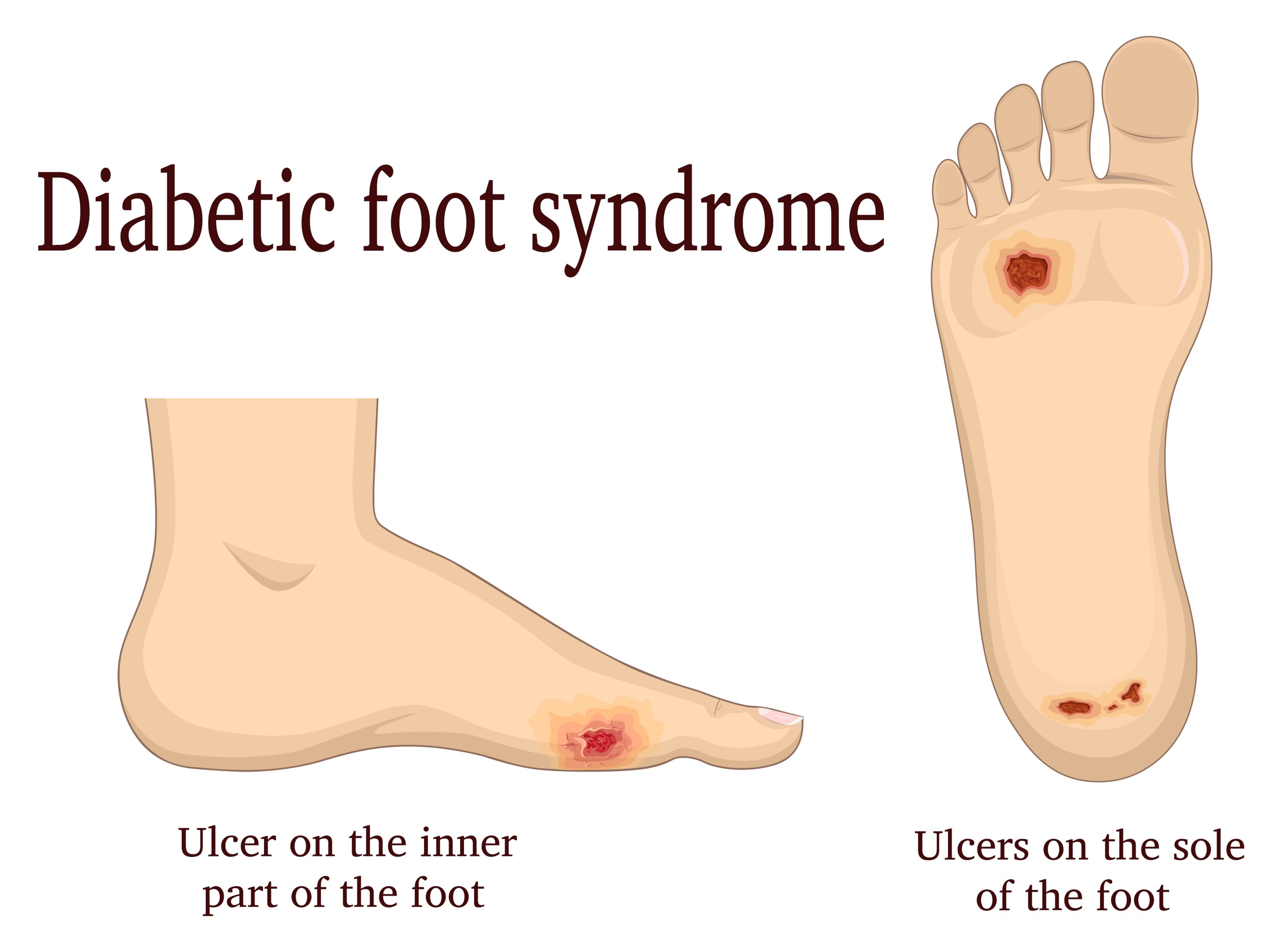
This medical-grade massager provides relief for tired feet, Plantar Fasciitis, Diabetics, and Neuropathy by increasing blood flow circulation. However, it is important to note that the Cloud Massage features varying levels of pressure, and we encourage you to use the lowest setting initially.
The Cloud Massage Shiatsu Foot Massager is a high-quality machine that you can feel the weighted quality of when you first open the box. The 100% no-hassle warranty is a testament to the confidence the company has in its product. We highly recommend giving it a try.

Adjustable Comfort Feature
At Cloud Massage, we understand that comfort is key when it comes to a foot massager. That’s why our massagers are designed to provide a deep kneading shiatsu massage at the optimum comfort angle, with an easily adjustable bar. Unlike other foot massagers that force you to keep your knees together and legs at a 90-degree angle, our adjustable comfort feature allows you to find the perfect position for your individual needs.
Our foot massager also features multiple settings for heat, air compression pressure, and vibration, providing the perfect massage for your feet, calves, toes, and ankles. The foot/calf area is 5″ wide and open-toed, 11″ long with air pressure cuffs deflated, ensuring that you get the most comprehensive massage possible.
Our medical-grade massager is designed to provide relief for tired feet, Plantar Fasciitis, Diabetics, and Neuropathy by increasing blood flow circulation. However, we do encourage you to use the lowest setting initially, as our massager features varying levels of pressure. If you experience slight soreness after the first few uses, don’t worry, this is normal and means that it’s working.
At Cloud Massage, we are proud to offer a 100% no-hassle warranty. You have nothing to lose, so why not add one to your cart now?

Dual Massage Feature
We were impressed with the Cloud Massage Shiatsu Foot Massager’s dual massage feature. It has multiple settings for heat, air compression pressure, and vibration, which provide the perfect massage for your feet, calves, toes, and ankles. The foot/calf area is 5″ wide and open-toed 11″ long with air pressure cuffs deflated.
The machine’s adjustable comfort angle allows for a deep kneading shiatsu massage at the optimum comfort angle, and it features an easily adjustable bar. Unlike other foot massagers that force you to keep your knees together and legs at a 90-degree angle, this one provides more flexibility.
The Cloud Massage Shiatsu Foot Massager is a medical-grade massager that increases blood flow circulation, providing relief for tired feet, Plantar Fasciitis, Diabetics, and Neuropathy. However, we caution users to use the lowest setting initially since the machine features varying levels of pressure. Most afflictions will feel slight soreness after an initial massage after the first few uses, which is normal and how you know it is working.
Overall, we found the dual massage feature of the Cloud Massage Shiatsu Foot Massager to be a standout feature that sets it apart from other foot massagers on the market.
Relief Feature
We were impressed by the Cloud Massage Shiatsu Foot Massager’s ability to provide relief for tired feet, Plantar Fasciitis, Diabetics, and Neuropathy by increasing Blood Flow Circulation. The medical-grade massager was able to knead deep into our tired feet, providing a soothing and relaxing massage.
We appreciated the adjustable comfort angle feature, which allowed us to customize the massage experience to our liking. Unlike other foot massagers that force you to keep your knees together and legs at a 90-degree angle, the Cloud Massage Shiatsu Foot Massager is adjustable and provides a comfortable massage experience.
The dual massage feature was also a standout. With multiple settings for heat, air compression pressure, and vibration, the Cloud Massage Shiatsu Foot Massager provides the perfect massage for our feet, calves, toes, and ankles. The foot/calf area was 5″ wide and open-toed 11″ long with air pressure cuffs deflated.
We did note that the Cloud Massage Shiatsu Foot Massager features varying levels of pressure, and we encourage users to start with the lowest setting initially. Most afflictions will feel slight soreness after an initial massage after the first few uses, which is normal and how you know it is working.
Overall, we were impressed with the Cloud Massage Shiatsu Foot Massager’s relief feature and would highly recommend it to anyone in need of a relaxing and rejuvenating foot massage.
Pros and Cons
After using the Cloud Massage Shiatsu Foot Massager for Circulation and Pain Relief, we found that it has many benefits. Here are some of the pros:
- Adjustable Comfort: The Cloud Massager provides a deep kneading shiatsu massage at the optimum comfort angle. The easily adjustable bar allows you to customize the angle and intensity of the massage to your liking. Unlike other foot massagers, you don’t have to keep your knees together and legs at a 90-degree angle, which makes it more comfortable to use.
- Dual Massage: The foot massager features multiple settings for heat, air compression pressure, and vibration. It provides the perfect massage for your feet, calves, toes, and ankles. The foot/calf area is 5″ wide and open-toed 11″ long with air pressure cuffs deflated.
- Relief: The medical-grade massager provides relief for tired feet, plantar fasciitis, diabetics, and neuropathy by increasing blood flow circulation. It helps to alleviate pain and discomfort in the feet and legs.
- Guarantee: The Cloud Massage machine is of high quality and durable. We are proud to offer a 100% no-hassle warranty. You have nothing to lose. Add one to your cart now.
While the Cloud Massage Shiatsu Foot Massager has many benefits, there are also some cons to consider:
- Varying Levels of Pressure: The foot massager features varying levels of pressure. We encourage you to use the lowest setting initially. Most afflictions will feel slight soreness after an initial massage after the first few uses. This is normal and is how you know it is working. However, some users may find the pressure too intense, which can be uncomfortable.
- Price: The Cloud Massage Shiatsu Foot Massager is a bit expensive compared to other foot massagers on the market. However, we believe that the quality and effectiveness of the product justify the price.
Overall, the Cloud Massage Shiatsu Foot Massager is a great investment for anyone looking for relief from foot and leg pain. The adjustable comfort and dual massage features make it a versatile and customizable option for different types of users. While the varying levels of pressure and price may be a concern for some, we believe that the benefits outweigh the cons.
Customer Reviews
We were curious to see what other customers had to say about the Cloud Massage Shiatsu Foot Massager. With over 14,000 ratings and an average rating of 4.4 stars, it’s clear that many people have found this product to be helpful.
Some reviewers mentioned that the massager can be intense, but that it’s effective at providing deep tissue massage for tired feet and calves. Others noted that it’s well-built and professional-looking and that it’s powerful enough to use on other parts of the body, like the calves.
While a few reviewers were disappointed with the product’s performance, most people seemed to find it helpful for relieving foot pain and discomfort. Overall, we think the customer reviews are a good indication that the Cloud Massage Shiatsu Foot Massager is a worthwhile investment for anyone looking for at-home foot massage therapy.
Conclusion
After using the Cloud Massage foot massager, we can confidently say that it is a great investment for anyone suffering from foot pain or looking for a relaxing massage. While some reviewers may have had mixed experiences, we found the machine to be sturdy and professional-looking, with a powerful motor that can be adjusted to suit different levels of intensity.
The massage felt deep and effective, and we noticed a significant improvement in our foot pain after just a few uses. The heat therapy was also a nice touch and helped to further relax our muscles.
Overall, we highly recommend the Cloud Massage foot massager for anyone in need of pain relief or relaxation. It’s a bit pricey, but we believe it’s worth the investment in the long run.
Frequently Asked Questions
What are the benefits of using a shiatsu foot massager?
Using a shiatsu foot massager has several benefits. It helps to relieve pain, reduce stress, and promote relaxation. The Cloud Massage Shiatsu Foot Massager is designed to provide a deep kneading shiatsu massage at the optimum comfort angle. It features an easily adjustable bar, which means you can adjust the angle of the foot massager to suit your comfort level. Unlike other foot massagers that force you to keep your knees together and legs at a 90-degree angle, the Cloud Massage Shiatsu Foot Massager allows you to adjust the angle of the massager to suit your comfort level.
How does the Cloud Massage Shiatsu Foot Massager compare to other foot massagers?
The Cloud Massage Shiatsu Foot Massager is one of the best foot massagers available on the market. It features multiple settings for heat, air compression pressure, and vibration, which means you can customize your massage experience to suit your needs. The foot/ calf area is 5″ wide and open-toed 11″ long with air pressure cuffs deflated, which means it can accommodate different foot sizes. The Cloud Massage Shiatsu Foot Massager provides relief for tired feet, Plantar Fasciitis, Diabetics, and Neuropathy by increasing Blood Flow Circulation. It is also FSA/HSA eligible, which means you can use your health savings account to purchase it.
What are the features of the Cloud Massage Foot and Calf Massager?
The Cloud Massage Foot and Calf Massager is designed to provide relief for tired feet and calves. It features multiple settings for heat, air compression pressure, and vibration, which means you can customize your massage experience to suit your needs. The foot/ calf area is 5″ wide and open-toed 11″ long with air pressure cuffs deflated, which means it can accommodate different foot sizes. The Cloud Massage Foot and Calf Massager is also designed to be easy to use. It features an intuitive control panel that allows you to adjust the settings with ease.
Is the Cloud Massage Foot Massager easy to use?
Yes, the Cloud Massage Foot Massager is easy to use. It features an intuitive control panel that allows you to adjust the settings with ease. The foot/ calf area is 5″ wide and open-toed 11″ long with air pressure cuffs deflated, which means it can accommodate different foot sizes. The Cloud Massage Foot Massager is also designed to be adjustable for your comfort level. It features an easily adjustable bar, which means you can adjust the angle of the foot massager to suit your comfort level.