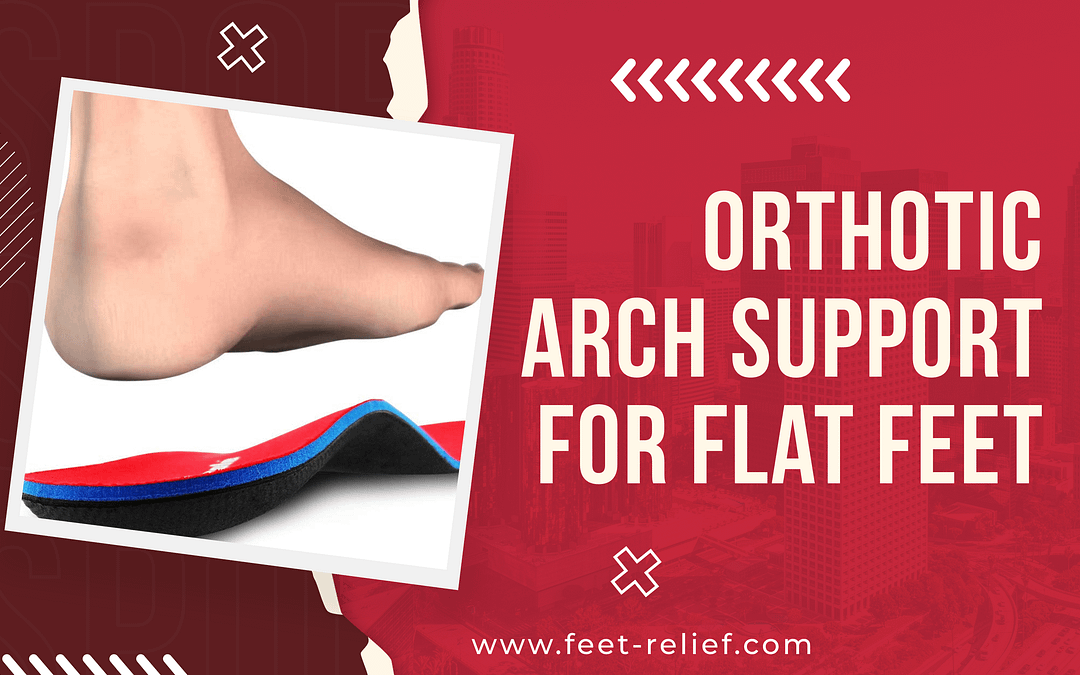
Orthotic Arch Support for Flat Feet
Flat feet can be a common problem that affects people of all ages. You may experience discomfort or pain in your feet, lower legs, and even your back if you have flat feet. The good news is that there are solutions to help manage the symptoms of flat feet, including the use of orthotic arch supports. In this blog post, we’ll take a deep dive into everything you need to know about orthotic arch support for flat feet.
We’ll discuss the anatomy of flat feet and their typical associated symptoms. Delving into the causes and risks of flat feet, we’ll explain how it can lead to injuries or complications. Then, we’ll explore how orthotics work and their benefits in managing flat feet.
Additionally, we’ll provide tips on selecting high-quality arch supports that fit well and are made from suitable materials. Finally, we’ll hear some personal testimonials from people who have used orthotic arch supports to manage their flat feet effectively and how they have benefited from using them. Keep reading!
Understanding Flat Feet
Flat feet, also called pes planus, occur when the foot’s arch collapses, leading to pain and fatigue in the foot, ankle, or lower leg. The arch provides shock absorption, support, and proper alignment for the body, making it crucial to understand your foot type for the right support. Physical therapy and supportive insoles help manage flat feet symptoms.
The Anatomy of Flat Feet
The arch muscles, tendons, and ligaments are critical for foot arch support, while the posterior tibial tendon can weaken in flat feet. The contours of your feet, leg alignment, and arch type all influence the foot’s arch. Genetic and developmental factors, as well as inflammation, can contribute to flat feet.
Typical Symptoms Associated with Flat Feet
Flat feet may cause pain, tenderness, or cramping in the inside of your ankle and the bottom of the foot. Individuals with this condition might experience foot fatigue, especially after extended standing or physical activity periods. Pes planus can lead to knee, hip, or back pain due to the extra strain on leg muscles.
Causes and Risks of Flat Feet
Genetic factors like tarsal coalition or rheumatoid arthritis contribute to flat feet, while lifestyle factors such as weight gain and high heels impact foot arches. Flat feet alter body alignment and can cause joint inflammation. Understanding these causes is crucial for effective treatment and support structure.
Genetic Factors
Abnormal bone fusion and tarsal coalition can contribute to flat feet due to genetic factors. Custom orthotics and supportive insoles are common management options for this condition.
Professional tests can detect the genetic predisposition for flat feet, aiding in effective management. Understanding these genetic factors is essential for comprehensive flat feet management.
Lifestyle Factors
Weight gain, hormonal changes, or pregnancy can contribute to flat feet. Prolonged use of high heels impacts arch support and may lead to flat feet. Lifestyle factors influence flexible flatfoot.
Proper support and shoe inserts alleviate discomfort. Understanding lifestyle impact guides appropriate support choices.
Flat Feet Injuries and Complications
Flat feet can lead to foot pain, arch pain, heel pain, or the development of plantar fasciitis. Long-term flat feet can cause extra strain on the legs, potentially leading to knee pain or hip pain.
Rigid flat feet may increase the risk of developing foot injuries or complications. Understanding potential injuries and complications is crucial for proper management.
The Link between Flat Feet and Back Pain
Flat feet alter body alignment, potentially causing lower back pain. The lack of arch support affects body weight distribution, leading to back pain.
Custom orthotics or supportive insoles provide relief. Addressing flat feet-related back pain often involves proper support and physical therapy. Understanding the connection is crucial for effective pain management.
The Role of Orthotics in Flat Feet Management
Orthotics, like supportive insoles or custom-made arch supports, offer optimal support for flat feet, realigning the foot and reducing strain while supporting the arch structure. They can alleviate pain, enhance foot function, and help prevent flat feet-related injuries. When combined with physical therapy, orthotics provide an effective approach to flat feet management.
How Orthotics Work
Orthotics function by providing the necessary support for arches in flat feet, ensuring proper alignment. These insoles offer shock absorption, stability, and relief from foot pain while evenly distributing body weight and reducing strain. Custom orthotics accommodate unique foot contours, maximizing effective foot pain management support.
Benefits of Orthotic Arch Supports
Orthotic arch supports offer relief for foot pain associated with flat feet, aiding in proper leg alignment and maximum arch support. These supports enhance shock absorption, reduce strain on leg muscles, and assist in weight distribution to prevent extra strain on the entire foot.
Selection Guide for Orthotic Arch Support
Consider the unique contours of your feet when choosing orthotic arch supports for maximum comfort and effectiveness. Look for options that provide proper leg alignment to support your body’s natural structure. Select arch supports that cater to your specific foot type and offer lower back, knee, and hip pain relief, effectively reducing foot fatigue and discomfort.
Material Considerations
Consider those with a deep heel cup for quality and support when choosing arch supports. For maximum comfort, look for rigid structures, counterarch supports, and supportive insoles.
Opt for flexible arch supports to relieve flat feet. Consider the material carefully to ensure proper support and relief.
Size and Fit Criteria
When selecting arch supports, ensure they fit your shoe size properly to provide effective support. Look for supports with arch muscle support for proper alignment and relief.
Check for arch support insoles and a high heel for proper alignment and pain relief. Opt for support that offers relief for joint inflammation caused by flat feet.
Where to Purchase Quality Orthotic Arch Support
When it comes to purchasing quality orthotic arch supports, online options provide convenience and a wide variety of sizes and designs. Physical stores offer the advantage of trying out supports before making a purchase and may even provide custom orthotics for proper relief. Consider options that cater to specific conditions like rheumatoid arthritis and plantar fasciitis.
Online Options
When seeking orthotic arch support online, consider customizable options for flat feet. Look for custom orthotics to provide proper support and relief, addressing foot fatigue, pes planus, tendons, and tarsal coalition.
Ensure the support structure caters to your specific needs, offering relief from common symptoms associated with flat feet. Tread Labs and Dash insoles are popular choices.
How to Use Arch Supports Effectively
Breaking in new orthotics is crucial for proper support and comfort. Maintenance tips are essential for prolonged use of orthotic arch supports for flat feet.
Proper arch supports relieve foot pain and provide support for flexible or rigid flatfoot. Consider arch supports that cater to different foot conditions and provide the necessary relief.
Breaking In Your New Orthotics
Adjusting to new orthotic arch supports for flat feet is crucial. Understand the process and follow guidelines for effective wear. Proper support is essential for foot pain relief.
Gradual wear maximizes support, promoting comfort. Breaking in your new orthotics ensures maximum benefit and relief.
Maintenance Tips for Prolonged Use
When using orthotic arch supports for flat feet, following maintenance tips for prolonged use and support is crucial. Proper care ensures long-term relief and foot health. Consider implementing best practices for cleaning and care to maintain the support structure and maximize the benefits of your arch supports.
Personal Testimonials of Orthotic Arch Support Users
Orthotic arch support has provided relief for foot and back pain, improved foot alignment, and reduced strain on leg muscles. It aids in shock absorption, offers comfort during physical activities, and relieves plantar fasciitis and heel pain. Many users have found significant benefits from the support structure offered by orthotic arch supports.
Can Orthotic Arch Support Completely Cure Flat Feet?
Orthotic arch support cannot completely cure flat feet, but it can provide pain relief and proper support for flexible flatfoot. It helps maintain leg alignment and supports the arch muscles for added stability, aiding in flat foot management. Additionally, it can help manage the common symptom of arch fatigue in flat feet.
Video Credit: @Footankle
Help with Foot Arch for Flat Feet
Orthotic arch supports can be highly beneficial for individuals with flat feet. These supports provide the necessary cushioning and support to alleviate pain and discomfort associated with this condition.
They help reduce foot fatigue and improve overall body alignment, reducing the risk of injuries and complications. When selecting orthotic arch supports, it is important to consider factors such as material, size, and fit to ensure maximum effectiveness.
Additionally, purchasing these supports from reputable sources, either online or physical stores, is advisable to ensure quality and authenticity. It is worth noting that while orthotic arch supports can greatly improve comfort and functionality, they may not completely cure flat feet. However, they can significantly enhance the quality of life for individuals with this condition.
If you are looking to find relief from flat feet and improve your foot health, consider incorporating orthotic arch supports into your daily routine. Don’t let flat feet hold you back from living an active, pain-free lifestyle.
Frequently Asked Questions
How can orthotic arch support help alleviate foot pain for those with flat feet?
Orthotic arch support is beneficial for individuals with flat feet as it helps redistribute pressure on the foot, providing relief from pain. It also adds stability to the foot and prevents overpronation.
Custom orthotics designed specifically for flat feet offer a personalized solution. Selecting comfortable and properly fitting arch supports is important for maximum benefit.
Are there different types of orthotic arch support available for flat feet?
Yes, there are many orthotic arch support options for flat feet. These include full-length insoles, 3/4 length insoles, and heel cups.
Custom-made orthotics are also available for individuals with severe flat feet or other foot conditions. It’s important to consult a podiatrist or healthcare professional to determine the best type of orthotic for your specific needs.
Can orthotic arch support be used in conjunction with other treatments for flat feet?
Orthotic arch support can definitely be used alongside other treatments for flat feet. These may include physical therapy, stretching exercises, and wearing supportive shoes.
Combining different treatments often leads to better results and increased comfort. Always consult a healthcare professional to determine the best treatment plan for your needs.
Learn What’s Best for Your Feet!
Learn what’s best for your feet with us! We offer an array of tips and tricks for foot care and relief.
For a deeper dive into foot health, visit our website: feet-relief.com.
Your journey towards happy, healthy feet starts here!