Feet-Relief is supported by our audience. When you purchase through one of our links, we may earn a small affiliate commission. As an Amazon Associate I earn from qualifying purchases.Your cost is not affected.
Exploring Strategies in Diabetic Foot Ulcer Prevention and Treatment
Imagine waking up one day and finding a wound on your foot that won’t heal. You try different remedies, but nothing seems to work. You start to feel pain, infection, and even gangrene. You are at risk of losing your foot, or worse, your life. This is not a nightmare, but a reality for millions of people with diabetes who suffer from diabetic foot ulcers (DFUs).
DFUs are one of the most serious and costly complications of diabetes, affecting up to 25% of diabetic patients in their lifetime. They can lead to amputation, disability, and death if not treated properly. However, DFUs are not inevitable. They can be prevented and treated with proper care and management. In this article, we will discuss what causes DFUs, how to prevent them, and how to treat them effectively.
We will also share some tips and resources to help you take care of your feet and avoid this devastating condition.
Understanding Diabetic Foot Ulcers
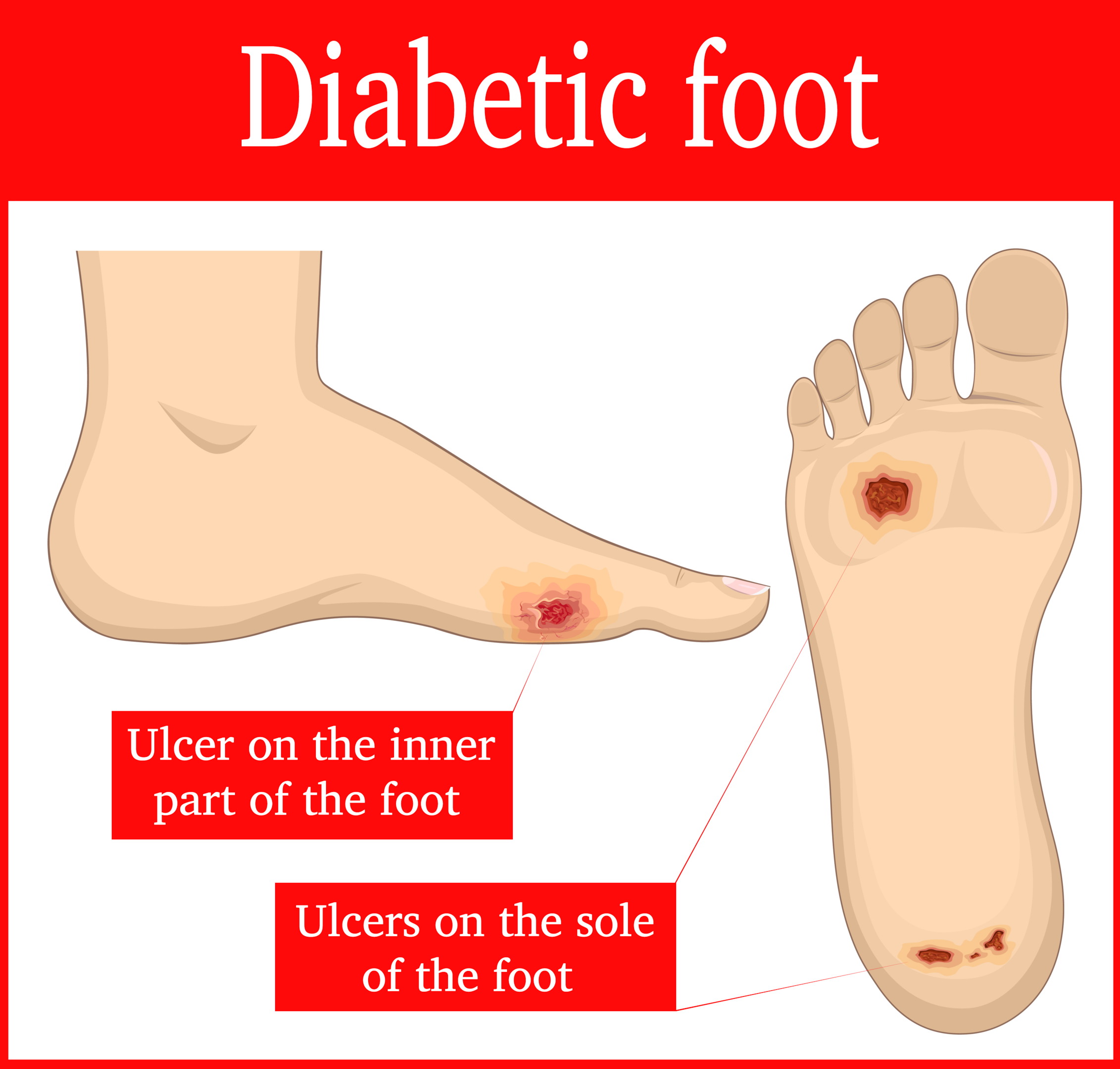
Diabetic foot ulcers are a common complication of diabetes, affecting up to a quarter of people with the disease. These are open sores or wounds that typically occur on the bottom of the foot and are a major cause of morbidity and disability. They occur due to a combination of factors including neuropathy (nerve damage), peripheral vascular disease (poor circulation), and infection.
Understanding the nature of diabetic foot ulcers
Understanding is the first step toward effective management. These ulcers develop from a minor wound that fails to heal due to the high blood sugar levels and impaired blood circulation characteristic of diabetes. Over time, this wound can become infected and develop into an ulcer, which can lead to severe complications if not treated promptly.
For those living with diabetes, knowledge about foot ulcers is crucial. It can help you identify early signs, take preventive measures, and seek immediate treatment when necessary. Moreover, understanding the full impact of diabetic foot ulcers can help you appreciate the importance of managing your diabetes well to prevent such complications.

Causes and Effects of Diabetic Foot Ulcers
The primary causes of diabetic foot ulcers include peripheral neuropathy and peripheral artery disease. Peripheral neuropathy, or nerve damage, often affects people with diabetes, leading to a loss of sensation in the feet. This means that minor cuts or blisters may go unnoticed and can escalate into a more serious wound or ulcer.
Peripheral arterial disease
Peripheral artery disease, on the other hand, affects blood flow to the feet. Poor circulation can hamper the healing of wounds and can also lead to the formation of ulcers. Other factors that can contribute to the development of diabetic foot ulcers include inappropriate footwear, trauma, and abnormal foot anatomy.
Effects of diabetic foot ulcers
The effects of diabetic foot ulcers are more than skin-deep. They can lead to severe infections that spread to the bone, resulting in a condition known as osteomyelitis. If not treated promptly, these infections can lead to gangrene and ultimately, amputation. Moreover, diabetic foot ulcers can significantly impact a person’s quality of life, leading to mobility issues, emotional distress, and financial burdens due to ongoing medical care.

Early Stage Diabetic Foot Ulcer: Signs and Symptoms
Recognizing the early signs and symptoms of a diabetic foot ulcer can be the difference between a manageable condition and a life-altering complication. The initial signs of a foot ulcer include swelling, redness, warmth, and pain in the affected area. You may also notice drainage in your socks or an unpleasant odor.
As the ulcer progresses, the skin around the wound may become calloused and hardened. The wound itself may deepen, and you may see an exposed tendon or bone. The pain may subside due to neuropathy, but the danger remains. An untreated foot ulcer can lead to serious infections and even amputation.
Being vigilant and proactive in monitoring for these early signs and symptoms can significantly reduce the risk of complications. It’s important to remember that not all foot ulcers cause pain, particularly in the early stages. Regular foot inspections are crucial, especially if you have neuropathy.

The Correlation Between Blood Sugar and Foot Ulcers
There’s a significant correlation between blood sugar levels and foot ulcers in individuals with diabetes. High blood sugar levels can damage nerves and blood vessels over time, leading to neuropathy and poor circulation — two key factors in the development of foot ulcers.
Elevated blood glucose levels
Moreover, high blood sugar can impede the body’s ability to fight off infections and slow the healing process. This means that even minor cuts or blisters can quickly escalate into a serious foot ulcer.
Keeping your blood sugar levels in check is therefore crucial in preventing foot ulcers. Good diabetes management, including regular monitoring of blood sugar levels and adhering to your prescribed medication regimen, can reduce the risk of foot ulcers and other complications.

How Diabetes Leads to Foot Ulcers
Diabetes is a complex disease that can lead to a variety of complications, including foot ulcers. This happens through a combination of neuropathy, poor circulation, and a weakened immune system.
Neuropathy results from high blood sugar levels damaging nerves, particularly in your legs and feet, leading to a loss of sensation. This means you might not feel a minor cut or blister, which can then worsen unnoticed.
Reduced blood flow adds to the problem
Poor circulation, another common issue in diabetes, means your feet may not get enough blood and oxygen, impairing the healing process. A weakened immune system means your body is less able to fight off infections, making it easier for a small wound to become a serious foot ulcer.
Strategies for Diabetic Foot Ulcers Prevention
Prevention is the best strategy when it comes to diabetic foot ulcers. This involves maintaining good blood sugar control, practicing good foot hygiene, wearing appropriate footwear, and having regular foot examinations.
Good blood sugar control is crucial in preventing nerve damage and poor circulation, two key factors in the development of foot ulcers. This involves adhering to your prescribed medication regimen, following a healthy diet, and regular exercise.
Good foot hygiene involves inspecting your feet daily for any cuts, blisters, or other abnormalities and washing them regularly with warm water and mild soap. It’s also important to keep your feet dry to prevent fungal infections, which can lead to ulcers.
Appropriate footwear provides protection against injuries and reduces pressure on certain areas of your foot. Regular foot examinations by a healthcare professional can identify potential issues before they escalate into a serious problem.
List of Steps to avoiding chronic diabetic foot ulcers
One of the best ways to avoid chronic diabetic foot ulcers (DFUs) is to prevent them from occurring in the first place. This can be done by following some simple steps to take care of your feet and control your blood sugar levels. Some of the steps are :
-
Check your feet every day for any signs of injury, infection, or abnormality.
Look for cuts, blisters, redness, swelling, or nail problems. Use a mirror or ask someone to help you if you have trouble seeing your feet.
-
Wash your feet every day with mild soap and warm water.
Dry them well, especially between the toes. Apply a moisturizer to prevent dryness and cracking, but avoid putting it between the toes.
-
Trim your toenails carefully and regularly.
Cut them straight across and file the edges. Do not cut them too short or into the corners. If you have difficulty trimming your nails, see a podiatrist or a foot care specialist.
-
Wear comfortable and well-fitting shoes and socks.
Avoid shoes that are too tight, too loose, or have seams or rough edges that can cause friction. Change your socks daily and choose ones that are made of cotton or other breathable materials. Do not walk barefoot or wear sandals or open-toed shoes that can expose your feet to injury.
-
Protect your feet from extreme temperatures.
Do not use hot water bottles, heating pads, or electric blankets on your feet. Do not expose your feet to direct sunlight or cold weather for long periods. Wear socks and shoes when going outside in cold or hot weather.
-
Control your blood sugar levels
Following your doctor’s advice on diet, exercise, medication, and monitoring. High blood sugar levels can damage the nerves and blood vessels in your feet, making them more prone to infection and slow healing. Keeping your blood sugar levels within the target range can help prevent or delay the onset of DFUs.
-
See your doctor regularly and have your feet examined at least once a year.
Your doctor can check for any signs of nerve damage, poor circulation, or other risk factors for DFUs. Your doctor can also provide you with education and guidance on how to prevent and treat DFUs effectively.
By following these steps, you can reduce the risk of developing chronic DFUs and improve your quality of life. Remember, prevention is better than cure when it comes to DFUs.
Treatment Options for Diabetic Foot Ulcers
When it comes to treating diabetic foot ulcers, the primary goals are to promote healing, prevent infection, and avoid amputation. This often involves a multidisciplinary approach including wound care, infection management, offloading (reducing pressure on the wound), and improving blood flow to the affected area.
Wound care involves regularly cleaning the ulcer and applying dressings to keep it moist and protect it from further injury and infection. Infection management may involve antibiotics if there’s an existing infection.
Offloading can be achieved through special footwear or devices that redistribute pressure away from the ulcer to allow it to heal. Improving blood flow to the affected area may involve medication or procedures to improve circulation.
Some of the common treatment options for DFUs are:
-
Wound care:
This involves cleaning and dressing the ulcer regularly to prevent infection and promote healing. The type of dressing used may vary depending on the wound characteristics and the doctor’s preference. Some examples of dressings are gauze, foam, hydrogel, alginate, or collagen.
Wound care may also include debridement, which is the removal of dead or infected tissue from the ulcer. Debridement can be done by surgical, mechanical, chemical, or biological methods.
-
Off-loading:
This means reducing or eliminating the pressure and friction on the ulcer by using devices such as casts, boots, crutches, or wheelchairs. Off-loading can help prevent further damage to the ulcer and speed up healing. Off-loading may also involve changing the footwear or orthotics of the patient to prevent recurrence of ulcers.
-
Medication:
This includes antibiotics to treat infection, painkillers to relieve pain, and anti-inflammatory drugs to reduce inflammation. Medication may also include drugs that improve blood flow or stimulate wound healing, such as pentoxifylline or platelet-derived growth factor. Medication may be given orally, topically, or intravenously, depending on the severity and type of infection.
-
Surgery:
This is usually reserved for cases where other treatments have failed or where there is a risk of complications such as gangrene or osteomyelitis. Surgery may involve removing part or all of the affected foot (amputation), grafting skin or tissue from another part of the body (skin grafting), or bypassing blocked arteries to restore blood flow (vascular surgery).
The treatment options for DFUs are not mutually exclusive and may be combined or modified according to the individual needs and preferences of the patient. The goal of treatment is to heal the ulcer as quickly and completely as possible, prevent recurrence and complications, and preserve the function and quality of life of the patient.
The Importance of Regular Foot Check-ups in Diabetes Management
Regular foot check-ups play a critical role in diabetes management. These check-ups allow healthcare professionals to identify any potential issues early and implement preventive measures before they escalate into serious complications such as foot ulcers.
During a foot check-up, your healthcare provider will look for any signs of neuropathy, poor circulation, and foot deformities. They will also check for any cuts, blisters, or other abnormalities that could potentially develop into an ulcer.
If you have diabetes, it’s recommended that you have a foot check-up at least once a year, or more frequently if you have a history of foot problems. These check-ups, along with ongoing foot care and good diabetes management, can significantly reduce the risk of foot ulcers and other complications.

Living with Diabetes: Tips to Prevent Foot Ulcers
Living with diabetes can be challenging, but with the right strategies, you can prevent foot ulcers and maintain your quality of life. Here are some tips:
- Keep your blood sugar levels in check. This is crucial in preventing nerve damage and poor circulation.
- Inspect your feet every day. Look for any cuts, blisters, or other abnormalities that could potentially develop into a foot ulcer.
- Wash your feet daily with warm water and mild soap, and keep them dry to prevent fungal infections.
- Wear appropriate footwear that provides protection and reduces pressure on your feet.
- Have regular foot check-ups. This allows healthcare professionals to identify any potential issues early and implement preventive measures.
Staying One Step Ahead of Diabetic Foot Ulcers
Diabetic foot ulcer prevention and treatment require a proactive and integrated approach involving good blood sugar control, regular foot care, and early detection. Understanding the causes and effects of foot ulcers can help you stay one step ahead and avoid the severe complications associated with this common diabetes complication.
Living with diabetes can be challenging. However, with the right strategies, patients with diabetes can maintain their quality of life and reduce the risk of foot ulcers. So, stay vigilant, be proactive, and always keep your foot health a priority.
In the journey of managing diabetes, remember, you’re not alone. Your healthcare provider is there to guide you, and there are numerous resources available to help you navigate this path. Keep learning, keep taking care of yourself, and most importantly, keep moving forward.
Amazon and the Amazon logo are trademarks of Amazon.com, Inc, or its affiliates.